At this year’s American Psychiatric Association (APA) Annual Meeting, I attended a panel titled “The Shame Train: How Shame Builds and Breaks Physicians and What We Can Do About It,” presented by psychiatry resident Dr. Kiera Benson and psychiatry attendings Dr. Carrie Dillon and Dr. Savannah Woodward. This session hit home in a way that few academic conference talks ever do.
They described how shame differs from guilt. Shame centers around the self — “I am bad” — whereas guilt is tied to behavior — “I did something bad.” For many in medicine, particularly trainees, this distinction is more than academic, it’s lived experience. When we fail a board exam, take a leave of absence, or fall short in professionalism, the system doesn’t just question our actions, it questions our worth.
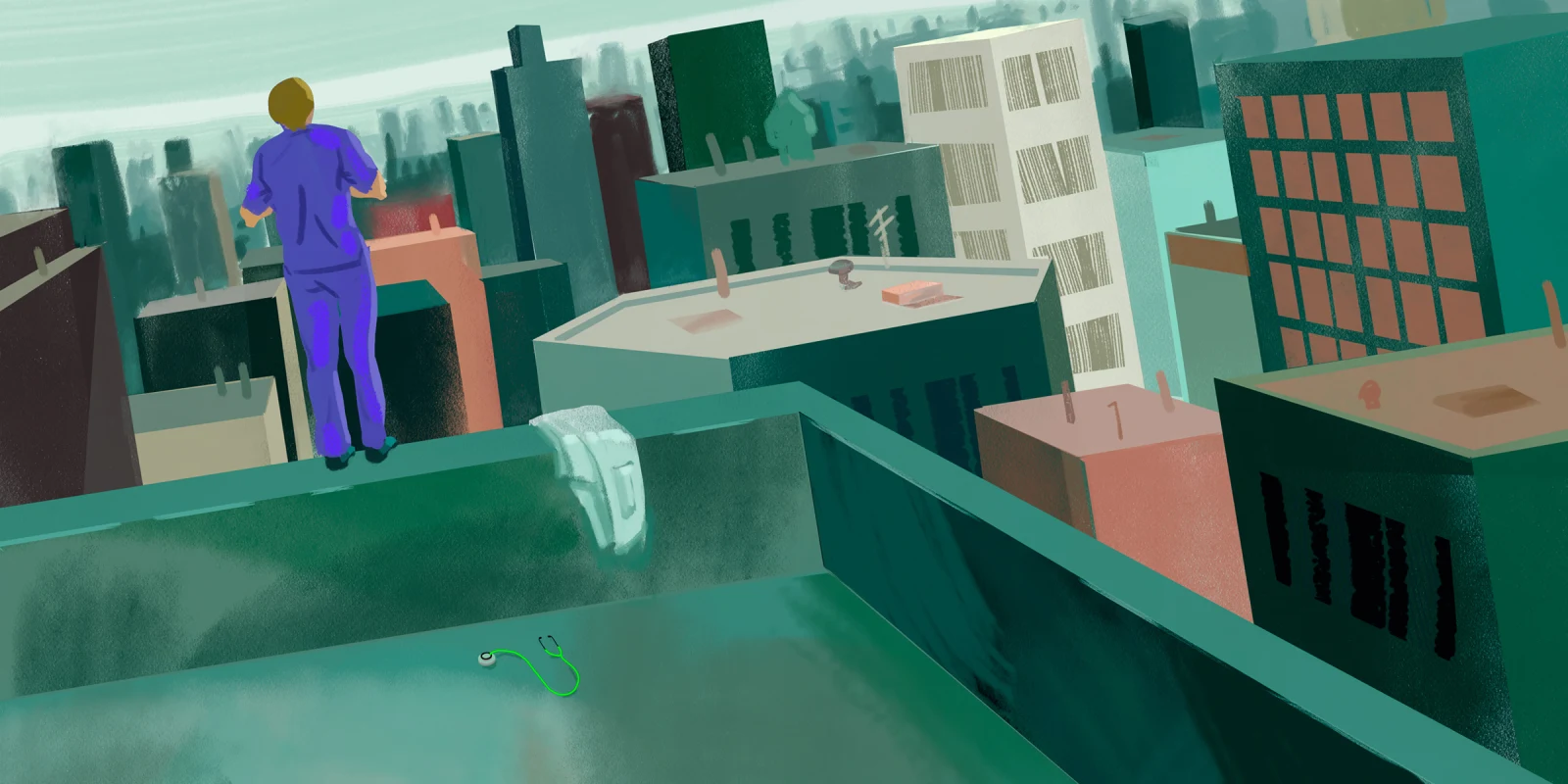
I know this because I lived it. I failed Step 1. Twice. I took a leave of absence (LOA). I was written up for professionalism. I’ve shared these stories before on Doximity in articles, and on podcasts, because silence helps shame thrive. When I failed Step 1, I truly believed my life in medicine was over. I contemplated suicide over a USMLE exam that I would eventually pass. That is the power of shame in medical education. That is the harm we do.
What could have been a growth moment was instead made into a moral failure. My administration withheld my ability to move forward with third-year rotations. When I asked for support or tried to find peers who had gone through similar struggles, I was met with ridicule. Not with compassion or guidance, and certainly not grace.
Through attending this APA session, I found words for what I and so many others have felt but couldn’t name: shame, isolation, and impostor syndrome. The medical student 2024 Graduation Questionnaire reveals how the fear of stigma around requesting help prevented students from asking for support from their institutions.
Let’s talk pathophysiology. Shame isn’t just an emotion; it’s a full-body stress response. It activates the sympathetic nervous system, including elevated cortisol and norepinephrine. Chronic exposure to this high stress has a consequence of impaired immunity, elevated blood pressure, and worsened mental health. Shame manifests cognitively and physically as rumination, tunnel vision, GI distress, panic, and worthlessness. Then, in far too many cases, shame leads to suicidal ideation.
Shame doesn’t affect everyone equally. As the APA panel pointed out, those most vulnerable are those already marginalized in medicine whether due to race, gender, disability, mental health history, or socioeconomic status. Our own APA Poster, “Navigating Leave of Absence in Medical School: Exploring the Impact on Underrepresented Students,” revealed that:
- 77% identified as underrepresented in medicine
- 70.7% identified as female and 48.7% as Hispanic/Latinx
- 51.7% reported they had a mental health condition
Furthermore, the culture of perfection in medicine compounds this, creating a toxic brew of overwork, self-neglect, and distorted identity. In our survey on medical students who took an LOA, 59% reported a shift in identity of being a medical student. Taking an LOA led 65% of these individuals to report feeling alone or very alone.
This isn’t just a medical education problem, it’s a public health one. Physicians have a significantly higher risk of suicide than any other field. It has been found that physicians who experience suicidal ideations (SIs) are less likely to seek support than those without SIs. It is imperative to de-stigmatize mental health support in the medical community.
The APA panelists hypothesized that this can be preventable if we start addressing shame early and openly in medicine. They emphasized that shame thrives in secrecy and seclusion. To overcome this shame we must provide connection, disclosure, peer mentorship, and community. This is why I created a peer group of students who had taken LOA or failed Step. Yes, I had to disclose my own story first, which was terrifying. However, with every disclosure, others quickly reciprocated the disclosure by stepping forward with their own stories of difficulty in medical education. Eventually, I spoke publicly through writing op-eds and sharing on social media and podcasts. I don’t blatantly encourage everyone to disclose publicly. However, I do strongly believe we should all feel safe enough to be human while in medical education.
As an incoming PGY2 psychiatry resident, I am the elected chief resident for medical student education and resident wellness at my program. In this role, I advocate not just for mental health but for a broader culture shift. One that is shame-informed, much like how we now promote trauma-informed care.
If you’re a resident, fellow, attending, or administrator, share your own challenges and failures. Debrief with compassion after a mistake is made, as mistakes are inevitable and just a demonstration of learning. Reject shame as a teaching tool, and foster communities of emotional support.
Shame is not a marker of weakness; it’s a response to unmet needs in a broken educational system. It is not a competency nor resilience training. Lastly, it is not the price we should be paying to become exemplary physicians.
We went into medicine to heal. Let’s not break each other along the way.
What would it take for you to openly address shame in medical training? Share in the comments.
Stephanie Moss, MD, a psychiatry resident, is dedicated to addressing mental health disparities and advocating for individuals with marginalized identities. She hosts the podcast "Life as a Patient-Doctor," which emphasizes the humanity in medicine. Dr. Moss is a 2024–2025 Doximity Op-Med Fellow. Connect with her @medpsycmoss on social media.
Illustration by Jennifer Bogartz