During the early part of the COVID-19 pandemic in 2020, my profession as a pediatric pulmonologist was intriguing to friends and family. They wanted to know how it was caring for kids with COVID-19. What was the atmosphere at the hospital? What was the trajectory of this virus? Physicians and other health experts were featured in the news to address questions from the public. My picture, along with those of other health care workers, was blown up into a life-size poster and placed on a light post along a major road in my town. I was branded a "health care hero," along with other physicians, nurses, and clinicians.
And then something happened. Within a year, physicians were met with jeering threats at fiery school board meetings, angry about masking. The public questioned the efficacy of vaccines. I did my due diligence reviewing the data that supported the efficacy and safety of vaccines, but I heard on more than one occasion, "Dr. Rao, I won't vaccinate myself or my child. I've done my own research."
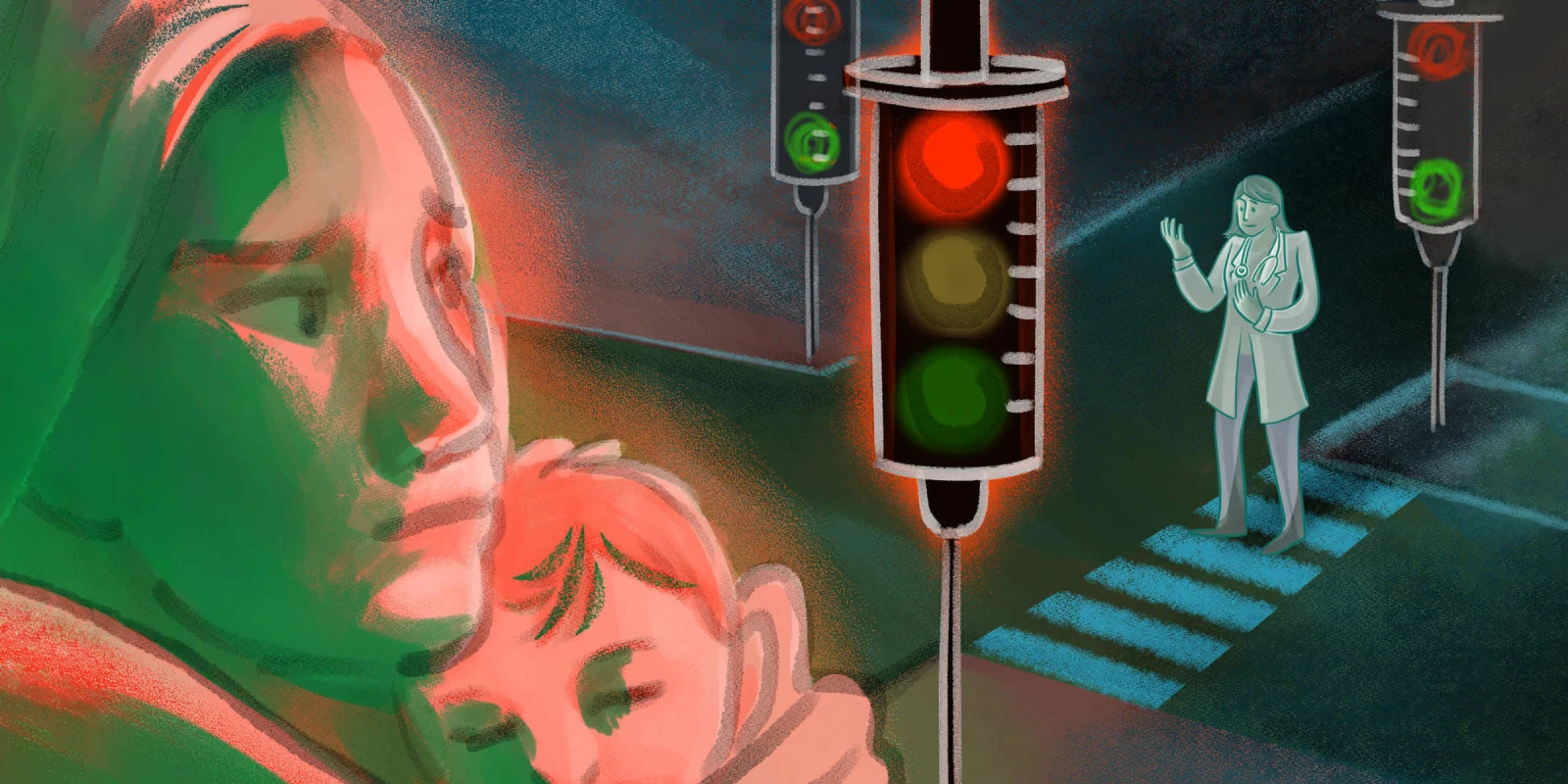
Increasingly, physicians encountered mistrust and were portrayed as agents of masking and chemical-laden medicines, all of which were categorized as "unnatural." In the public imagination, "natural" became the preferred antithesis to science and a way to achieve optimal health. In the process, the narrative that physicians work in the best interest of patients was maimed.
The main victim of this narrative has been patients. A prime example is the most recent influenza season, which was estimated to be one of the worst experienced by children. Influenza vaccine rates for children in the 2024-25 season dropped to 49.2%, representing an over 13% decline compared to pre-pandemic vaccination rates. The 2024-25 influenza season also had the highest number of pediatric deaths ever recorded, at 216, despite the high effectiveness of the influenza vaccine.
Experts believe that reduced vaccination rates, in part, contributed to more severe influenza disease. This vaccine hesitancy is a reflection of mistrust in science and stems from a narrative that has been twisted. Now, physicians have become suspicious wardens of chemical, "unnatural" medicine, and the public increasingly doesn't want any part of it.
The funny thing is, as a physician, I also value "natural" methods. I encourage my patients to eat fresh fruits and vegetables, get regular sleep, take vitamin D, breathe fresh air, limit their intake of processed foods, and reduce screen time — habits that pediatricians have advocated for decades.
However, somewhere along the way, the word "natural" was co-opted to mean "anti-science." I recently saw a young girl with severe asthma whose grandmother proudly shared that she'd switched to a "natural" (and expensive) allergy medicine, only for us to discover the medicine contained loratadine, the active ingredient in a common over-the-counter antihistamine. She was surprised at how she was misled and was grateful that I pointed out the ingredients. Another parent, after firmly refusing the COVID-19 vaccine despite my sharing the data, was hospitalized with COVID-19 and expressed to me that he wished he had gotten the vaccine earlier, as I advised. On a less extreme level, I have cared for countless families whose children sleep better when TVs are removed from bedrooms, and when a little guided meditation is used before bedtime, with or without melatonin.
We all have stories of when we used "natural" methods rooted in science, sometimes in combination with modern medicine, and where "natural" medicines have failed patients. We need to tell these stories to show that the divide between "natural" and "scientific" is artificial, and that the right medicine is the one that helps our patients thrive.
Physician storytelling has a rich history, inviting the world to view life and death from our unique perspectives. Through storytelling, we invite our readers and listeners into a world of human suffering, which we strive to alleviate and address. We can follow in the footsteps of fellow physicians who have led the way, including William Carlos Williams, Abraham Verghese, and Danielle Ofri. These are all physician authors with published books, including both fiction and nonfiction works.
Alternatively, we can share our stories in a modern way. Kimberly Manning, for instance, shares her stories by treating underserved patients on social media and through a podcast. Dr. Glaucomflecken tells his stories through the lens of comedy through TikTok and other platforms, while shedding light on unjust health insurance policies. There are numerous physicians building social media platforms and blogs, and there is evidence that storytelling may promote physician well-being.
We must share our stories of children vaccinated against influenza who present to our offices in significantly better health than those who were not vaccinated. We must share the stories of patients whose asthma improves with life-changing biologic medications. We need to share stories about our patients and their families who express gratitude for our efforts, such as when a child's asthma improved after we wrote a letter to the landlord requesting pest control services. Stories like the parent of a child with asthma who, after years of hearing me discuss the harms of second- and third-hand smoke, tells me they've smoked their last cigarette. These are the patient stories that do not make it through the filtered lens of headlines and clickbait. These are my stories as a pediatric pulmonologist that motivate me to continue to practice in a world where "natural" is wrongly pitted against modern medicine.
During the early days of the pandemic, physicians were celebrated as heroes. But over time, our clinical expertise became entangled within a cultural backlash against modern medicine, and "natural" approaches were seen as the preferred and safer alternative. The truth, however, is more complex. Physicians have long encouraged a foundation for health based on natural principles: nutrition, movement, rest, and connection. We also know that modern tools, such as vaccines and biologics for asthma, can save lives. The idea that we must choose between one and the other does a disservice to our patients.
This is why we must tell our stories as physicians that reaffirm our position as stewards of health. These stories can remind the public and ourselves that science is not opposed to nature, but rather serves as a tool for patients to live their best lives. Storytelling helps physicians reclaim that truth, rebuild trust, and affirm why our voices still matter.
How has sharing your experiences as a physician helped your patients? Share below.
Devika Rao is a practicing pediatric pulmonologist in Texas. She enjoys writing, trying new vegetarian recipes, yoga, and spending time with her two boys and husband. Dr. Rao was a 2024-2025 Doximity Op-Med Fellow.
Illustration by April Brust