I walked into the 2026 ACTRIMS Forum in San Diego with the same question I carry into the clinic every week: why do so many of my MS patients still progress and report ongoing symptoms, even when their MRIs look quiet? Progression is not uncommon in MS; an evolving paradigm is how to detect it earlier and earlier. By the end of three days, the field had handed me a paradigm shift: one that may finally let us treat the biology driving disability, not just the relapses we can see.
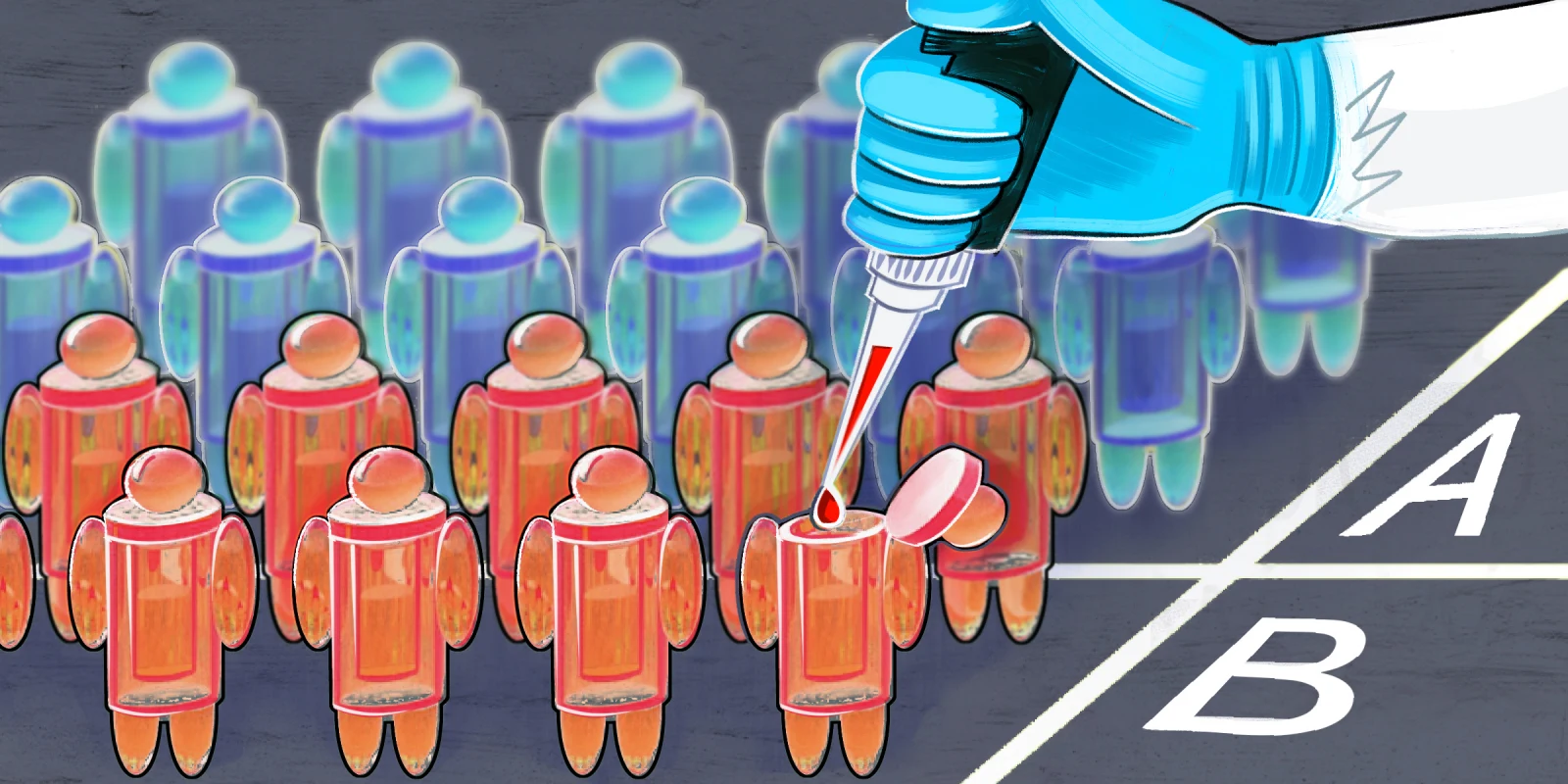
This year’s meeting revolved around a unifying theme: moving from symptom surveillance to biology-driven precision. Across plenaries, late-breaking trials, and mechanistic deep dives, the message was consistent: use of advanced biomarkers, CNS-penetrant therapies, and emerging interventions aimed at neuronal resilience may define the next decade of MS care.
On the first day, Dr. Jeffrey Cohen from Cleveland Clinic opened with his Kenneth Johnson Memorial Lecture on autologous hematopoietic stem cell transplantation (AHSCT), reminding us that with the EBMT registry now tracking more than 2,200 patients and treatment-related mortality below 0.3%, AHSCT has quietly evolved from experimental to carefully considered for highly active relapsing MS. Yet Cohen was refreshingly candid about what we still don’t know: ideal conditioning intensity, patient selection beyond “young and aggressive,” and long-term survivorship data remain open questions. The BEAT-MS trial may help answer whether AHSCT can outperform best-available high-efficacy therapies, but as Cohen noted, implementation challenges around coordination, cost, and access loom. For those of us at smaller centers, AHSCT still feels aspirational, and the science is still far from perfect.
On day two, Manuel Friese’s Barancik Prize lecture reframed progression as something deeper than immune attack: a neuron-intrinsic vulnerability that smoldering inflammation exploits. His group’s work on the neuronal immunoproteasome, metabolic shifts, and complement factor H as a resilience axis was a stark reminder: even perfect peripheral immune control may not be enough if neurons remain metabolically fragile. These mechanisms have evolved to protect the brain against infections and stressors as a high-stakes site and remind me that we have yet to discover so much about neurons and their metabolism. He also shared early case reports of CD19 CAR-T in MS (both progressive and relapsing phenotypes), where CAR-T cells were detected in CSF and intrathecal oligoclonal bands fell — hinting at compartment access that our modern monoclonals may not achieve. But new lesions during follow-up underscored how much we’re still learning about tissue-level biology. Maybe it is about the cells penetrating lesions, or maybe there are breakthrough relapses; only time will tell. It was equal parts thrilling and humbling.
If there was a unifying thread across sessions, it was the elevation of fluid biomarkers from research curiosity to clinical decision tool — and a frank acknowledgment that current trial endpoints need refinement. Multiple sessions questioned whether whole-brain atrophy is sufficient as a primary outcome, highlighting pseudoatrophy, age-related confounding, and insensitivity to compartmentalized tissue loss. The call was clear: we need sharper imaging biomarkers and analytic approaches to separate true neurodegeneration from inflammatory and aging noise. For those of us who have watched trials fail on atrophy endpoints despite clinical signals, this felt validating. Another standout was a session on astrocyte biology, particularly the role of proteins like Hevin in synaptic pruning and plasticity. It’s a reminder that MS pathology isn’t just about what immune cells do to the brain, but how resident CNS cells respond and sometimes betray the neurons they’re meant to support.
A highly anticipated topic was GLP-1 receptor agonists as potential add-on neuroprotective therapy. Personally, some MS specialists (including myself) have started prescribing these therapies to help brain health and are seeing real-world changes in terms of disability and fatigue. Although recent Alzheimer’s and Parkinson’s trials showed no benefit on primary cognitive endpoints, exploratory CSF biomarker signals and preclinical MS data with the CNS-penetrant analogue NLY01 have fueled cautious optimism. A new trial is now recruiting MS patients on ocrelizumab with and without GLP-1RA co-treatment — a pragmatic test of whether metabolic modulation can complement immunotherapy. It’s the kind of repurposing bet that feels very 2026: CNS-active, and potentially neuroprotective. I’m watching this one closely.
The meeting’s most clinically consequential moment was the FENtrepid results: fenebrutinib met non-inferiority to ocrelizumab in primary progressive MS at 12 weeks — the first new option in over a decade. A 12% numerical reduction in disability progression with early curve separation and a striking 22% post-hoc benefit on a composite including upper-limb function (9-Hole Peg Test and EDSS) suggests that oral, brain-penetrant BTK inhibition may offer a mechanistic edge by targeting both peripheral B cells and CNS-resident microglia. Hepatic safety signals (transient transaminase elevations in 13%) will require vigilance, but the promise of a CNS-penetrant oral agent feels paradigm-shifting. The PERSEUS trial using tolebrutinib in secondary progressive MS was disappointing by comparison, underscoring real intra-class variability in BTK inhibitor mechanisms.
Another highlight was obexelimab, a bifunctional antibody that co-engages CD19 and the inhibitory FcγRIIb receptor. Unlike anti-CD20 therapies, obexelimab doesn’t eliminate B cells — it “turns down the volume” on activation while preserving the cellular compartment. In the phase 2 MoonStone trial of relapsing MS, weekly subcutaneous obexelimab achieved about a 95% relative reduction in new gadolinium-enhancing lesions by weeks 8–12. For a field increasingly worried about deep hypogammaglobulinemia in long-term CD20 users, this modulation-rather-than-depletion approach is intriguing. Final 24-week data are due in 2026, and I suspect they’ll shape how we think about sequencing and de-escalation.
Leaving San Diego, I’m struck by how much the field has matured. The next frontier isn’t simply more immunosuppression; it’s smarter intervention and targeted CNS protection.
As the field evolves, I am most excited about pairing CNS-penetrant therapies with neuroprotective strategies and using advanced testing to guide escalation before MRI or EDSS catch up. Several sessions challenged us to rethink trial design entirely, moving from “did the lesion count drop?” to “did we preserve what matters: cortical integrity, synaptic reserve, and the capacity for repair?” The key is to start embracing these factors early in our clinical diagnostics and treatments. Hopefully, the next ACTRIMS-ECTRIMS combined meeting in 2026 will decipher more science about our understanding of MS and personalized and targeted DMTs.
Dr. Gupta has received grants from EMD Serono, the Child Neurology Foundation, and the Norton Foundation.
Illustration by April Brust