Hormone Receptor (HR) positive Breast Cancer
Advanced Disease
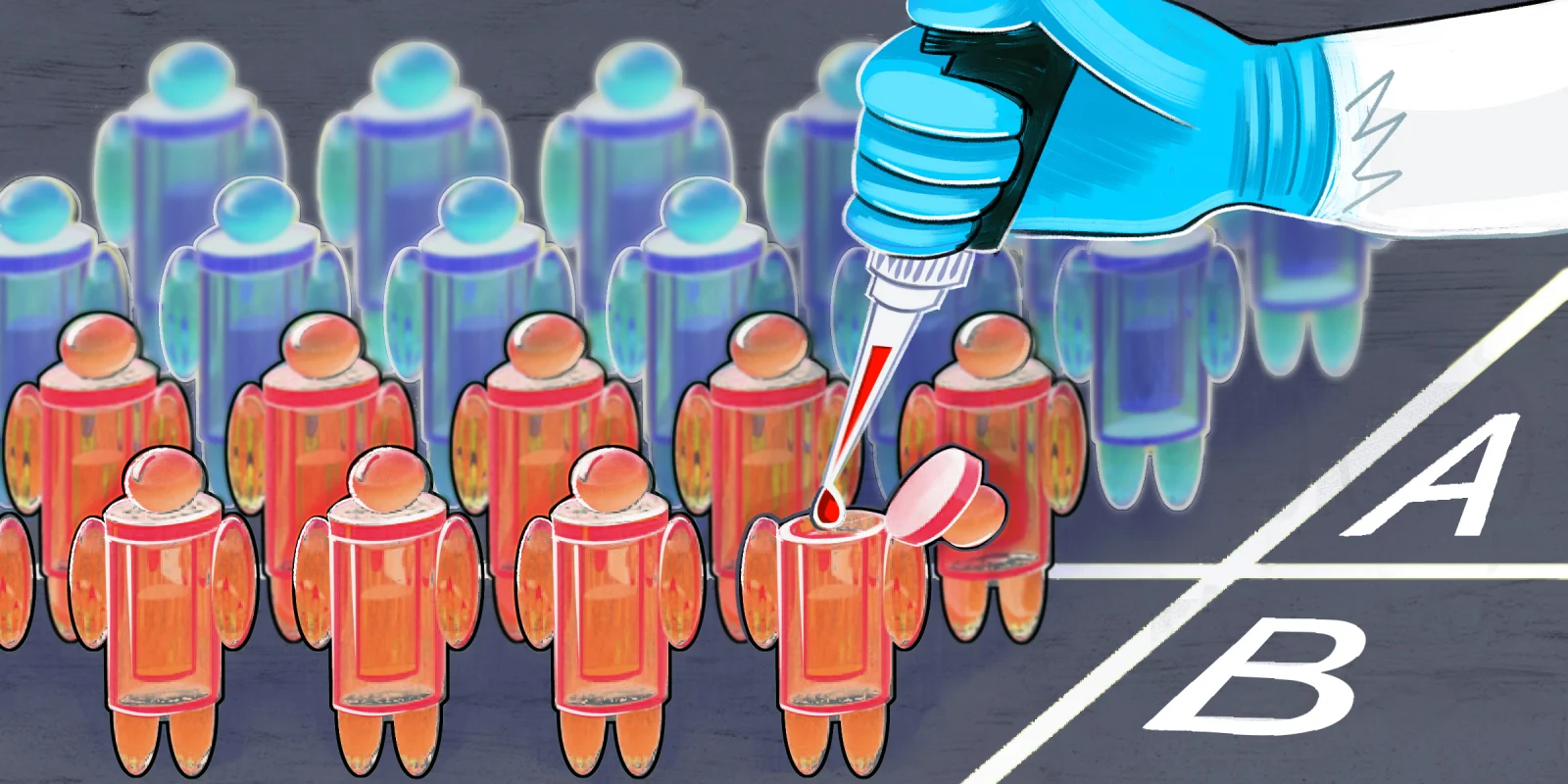
CDK4/6 inhibitors combined with endocrine therapy (ET) remain the gold standard for first line treatment of HR positive HER-2 negative advanced breast cancer (ABC), but what are the best treatment options for patients at the time of disease progression, in the absence of an actionable mutation (e.g. PIK3CA)? At SABCS 2022, Dr. Mayer presented the results of the PACE study (a randomized phase II study) which demonstrated that continuing treatment with palbociclib, a CDK4/6 inhibitor (> 85 % on Palbociclib first line), at disease progression in combination with fulvestrant did not result in better clinical outcomes vs fulvestrant alone (median progression free survival 4.8 and 4.6 months respectively). Interestingly the addition of the PD-L1 inhibitor, avelumab, to palbociclib and fulvestrant resulted in improved PFS and overall survival suggesting further exploration of this triplet is warranted.
A number of oral selective estrogen receptor down regulators (SERDS) are being evaluated in patients who progress on CDK4/6 inhibitors. Updated results from the EMERALD study, a phase III study of the next generation oral SERD, elacestrant vs standard of care (fulvestrant or an aromatase inhibitor) in the 2nd line setting, demonstrated that longer duration of CDK 4/6 inhibitor in the first line setting was associated with longer progression-free survival (PFS), particularly in the setting of an ESR1 mutation where patients who had a least 12 months of a CDK 4/6 inhibitor had a median PFS of 8.6 months vs 2.1 months in the standard of care (SOC) arm. The results of SERENA-2, a randomized phase II study of a next generation oral SERD and pure estrogen receptor antagonist camizestrant, was presented by Dr. Oliveira. Patients with HR positive HER-2 negative ABC were randomized to one of 3 doses of camizestrant (75/150/300 mg(dropped early)) vs fulvestrant after failure of 1st line therapy (50 % exposed to prior CDK4/6 inhibitors). At a median duration of 16-17 months follow-up the median PFS was statistically and clinically improved: 7.2 months (75 mg arm); 7.7 months (150 mg arm) vs 3.7 months with fulvestrant. Unique toxicities (all grade) with camizestrant (150 mg dose) included photopsia (24.7 %) and sinus bradycardia (26.0 %). Two phase III trials (SERENA-4 and 6) are on-going with camizestrant at the 75 mg dose.
Dr. Turner presented the results of the CAPItello-291, a phase III trial of capivasertib (a selective inhibitor of AKT isoforms 1/2/3) and fulvestant vs fulvestrant alone in patients with HR+/HER2- ABC who had up to 2 prior lines of endocrine therapy. There was a statistically and clinically meaningful benefit for patients treated with capivasertib and fulvestrant (median PFS 7.2 months) vs fulvestrant alone (3.6 months) HR = 0.60 p < 0.001. Clinical benefit was maintained in patients regardless of AKT mutation status as well as for those previously treated with CDK4/6 inhibitors (70 %). All grade diarrhea was more pronounced in the combination arm (72.4 %) compared to fulvestrant alone (20 %). Overall survival data is still immature.
Early-Stage Disease
For women with HR positive/HER-2 negative early-stage breast cancer (ESBC) 5-10 years of ET remains standard of care. Updated results of MONARCHE confirmed the clinical benefit of the addition of 2 years of abemaciclib to endocrine therapy in the setting of high risk disease – 4 or more lymph nodes (LN) positive or 1-3 LN positive and grade 3, or tumor > 5 cm or high risk based on Ki-67 (≥20%). At a median of 42 months follow-up, there were fewer invasive disease free survival events in the combination arm vs endocrine therapy alone (336 vs 499; HR 0.664; p< .001). While overall survival data remains immature, there was a 6.4% absolute benefit at 4 years in the abemaciclib plus endocrine therapy arm. Interestingly, while Ki-67 was prognostic, it was not predictive of benefit. We await the results of the NATALEE study, which randomized women to 3 years of ribociclib and endocrine therapy vs endocrine therapy alone in a similar patient population.
For young women with HR positive ESBC, 5-10 years of ET can limit fertility options due to increasing maternal age. The POSITIVE trial presented by Dr. Partridge, demonstrated that interruption of ET (after 18-30 months for up to 2 years), to conceive a child, did not negatively impact the breast cancer free interval at a median of 41 months. Although longer follow-up is needed these results are encouraging, providing women and health care providers with some reassurance that pausing endocrine therapy to pursue pregnancy does not appear to have a negative impact on breast cancer outcomes.
HER-2 positive Advanced Breast Cancer
At SABCS 2022, updates on the clinical benefit of trastuzumab deruxtecan (T-DXd) in HER-2 positive ABC were presented, solidifying the role of T-DXd in the second line setting. An updated analysis of DESTINY-BREAST03, comparing T-DXd to trastuzumab emtansine (T-DM1) reported overall survival (OS) data and updated progression-free survival (PFS) and safety data. With a median follow-up of 28.4 months (T-DXd) and 26.5 months (T-DM1), OS was 94.1% (T-DXd) vs 86% (T-DM1) at 12 months and 77.4% (T-DXd) and 69.9% (T-DM1) at 24 months. Median OS was not reached but the prespecified boundary for OS was crossed (P=0.013). Updated median PFS was 28.8 months (T-DXd) vs 6.8 months (T-DM1). Interstitial lung disease (ILD) occurred in 15.2% (T-DXd) vs 3.1% (T-DM1) though no grade 4 or 5 events reported. DESTINY-BREAST02 compared T-DXd to physician’s choice (TPC) (trastuzumab + capecitabine or lapatinib + capecitabine) in patients treated previously with T-DM1. Median treatment duration was 11.3 months (T-DXd) vs 4.5 months (TPC) and there was statistically significant improvement in both PFS and OS vs TPC. Overall response rate (ORR) was 69.7% (T-DXd) vs 29.2% (TPC). ILD was seen in 10.4% of patients, with two grade 5 events. DESTINY-BREAST09 is on-going and will determine the clinical benefit T-DXd vs T-DXd with pertuzumab vs SOC in the first line setting.
Dr. Dent and Dr. Moore do not have any conflicts of interest to report.
Illustration by April Brust