The American College of Rheumatology meeting that was held in Philadelphia this November is always a place to learn the latest cutting-edge concepts and treatments in rheumatology. Rheumatologists from around the world gathered to share their data. One presentation that was eye-opening was the use of a checkpoint inhibitor agonist to treat rheumatoid arthritis (RA), presented by Professor Paul Emery of the University of Leeds, UK. Peresolimab binds to programmed cell death protein 1 (PD-1), a checkpoint inhibitory receptor, and stimulates immune inhibitory pathways to restore immune homeostasis. This study showed statistically significant improvement by DAS28-CRP in the peresolimab groups (300 mg or 700 mg) every 4 weeks intravenously vs placebo. Of particular significance was the similar efficacy of peresolimab in those with prior exposure to DMARDs. This is always a difficult-to-treat group as the best response in studies is always those without prior treatment. This gives hope that peresolimab might be effective in these treatment resistant patients. Specific data on safety was not presented but the treatment of emergent adverse events were similar in all groups and no one in the high dose peresolimab group discontinued treatment due to adverse events. This was a phase IIA study, and we will have to wait for further data to see if this new mechanism of action will be added to the rheumatologist’s toolbox for RA in the future.
Sjögren’s Syndrome (SjS) is an orphan disease. It is very common with one study estimating an incidence of 3 million in the US versus 1 million for SLE. There are no FDA approved drugs for SjS. Professor Thomas Dörner of the Charité Universitätsmedizin in Berlin presented phase II results of a potent oral Bruton tyrosine kinase (BTK) inhibitor, remibrutinib, in moderate to severe SjS. BTK is expressed in cells of both the adaptive and innate immune systems including B cells and is a key component for B-cell receptor and Fc receptor signaling. This was a 24-week safety and efficacy study. There was significant improvement in the EULAR Sjögren’s Syndrome Disease Activity Index (ESSDAI) in the treated groups. Salivary flow increased (though not statistically significant) and total serum IgG and IgM decreased from baseline but remained in the normal range in those receiving remibrutinib. Infection was the most common AE in the treated groups and placebo with similar AE event rates in all 3 groups. It is encouraging that Sjögren’s Syndrome is now on the radar of investigators and new therapies are being developed.
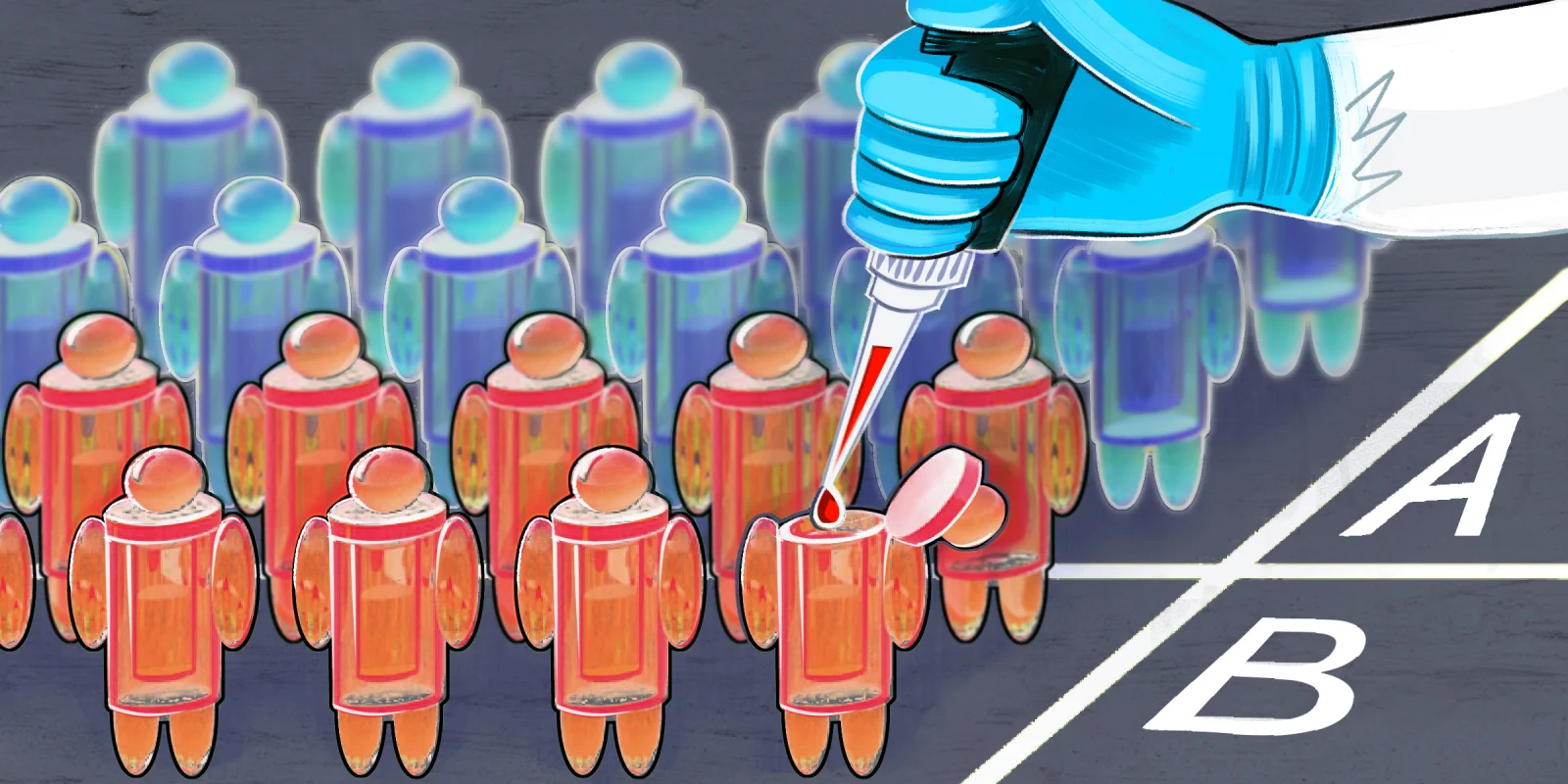
Another abstract that caught my attention was “Chimeric Autoantigen-T Cell Receptor (CATCR)-T Cell Therapies to Selectively Target Autoreactive B Cells.” In this study, presented by Maximilian F. Konig of Johns Hopkins, the investigators noted that CD19-targeted CAR-T cells hold promise for the treatment of refractory autoimmune diseases, but that indiscriminate depletion of all B cells can lead to infection. The present study utilized targeted CATCR-T cells to selectively kill anti-Beta-2 Glycoprotein I (B2GPI) B cells in antiphospholipid syndrome (APS). The authors described a precision cellular immunotherapy approach for the autoantigen-specific depletion of autoreactive B cells in autoimmune disease that holds promise of treating autoimmunity without increasing the risk of infection. While this was a “bench” study, it demonstrates what may be the future of rheumatology.
Dr. McLain has no conflicts of interest to report.
Illustration by April Brust