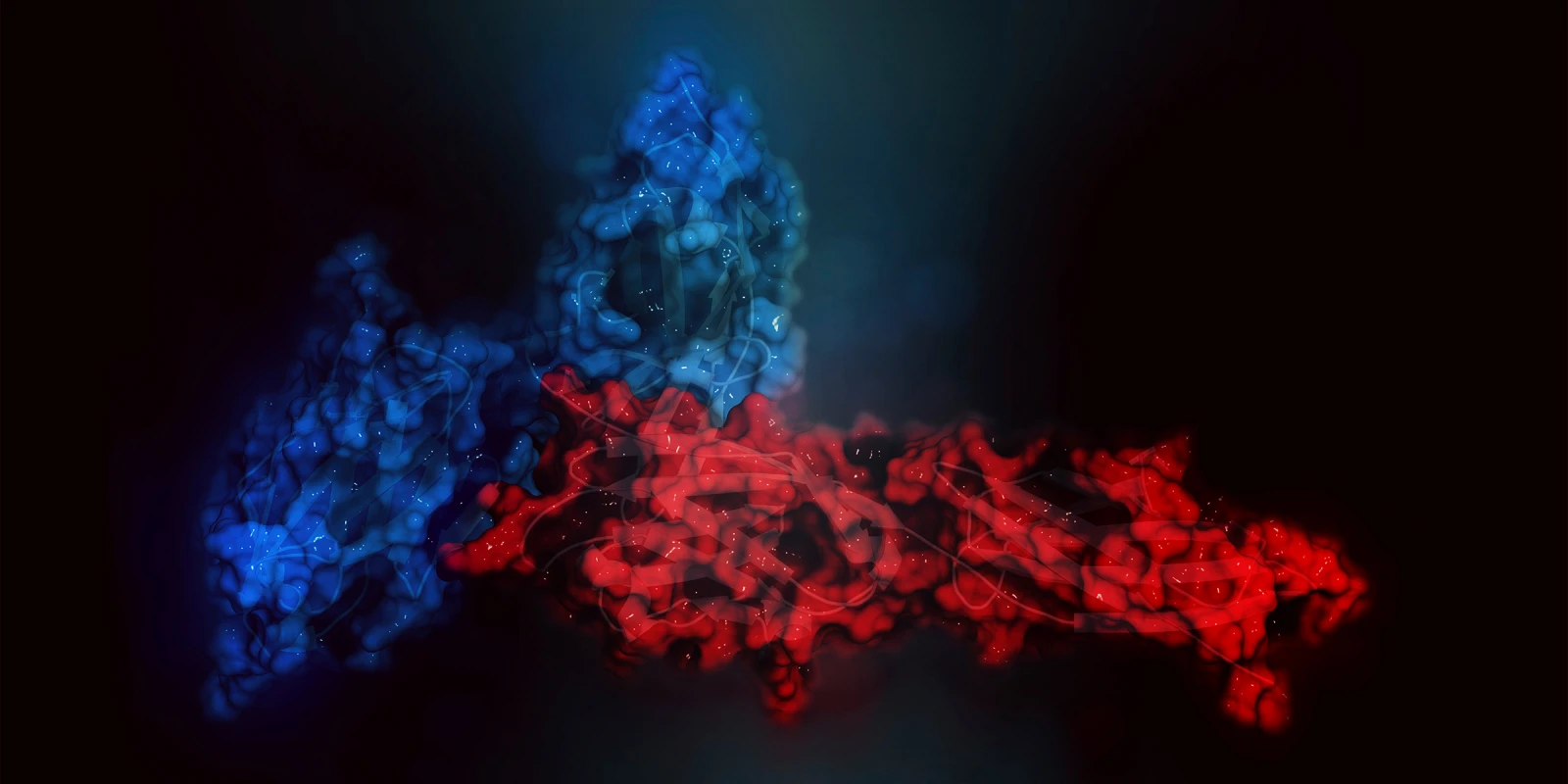
Cancer immunotherapy works by restoring the patient’s anti-tumor immunity to fight cancer. Cancer immunotherapy is considered a breakthrough in the fight against cancer. Checkpoint inhibitors are a form of cancer immunotherapy and have revolutionized treating advanced head and neck cancer (HNC). Advanced HNC is often associated with a poor prognosis and low survival rates. Pembrolizumab is a cancer immunotherapy that binds to — and blocks — the programmed cell death protein 1 (PD-1) on immune cells. Normally, PD-1 expressed on immune cells binds to programmed cell death ligand 1 (PD-L1) located on normal cells within the body. In this way, PD-1 protects the body from the immune system attacking the body’s cells, and therefore is considered an “immune checkpoint.” Cancer cells can express PD-L1, which binds to the PD-1 on immune cells and prevents the immune cell from killing the cancer cell. In this way, the cancer cells can “hide” from the immune system.
When pembrolizumab was FDA approved for the treatment of refractory recurrent and metastatic HNC in 2016, it became the first new therapeutic agent for the treatment of HNC in a decade. In 2019, the findings from the KEYNOTE-048 trial — a phase III clinical trial — established pembrolizumab as first-line therapy for patients with unresectable recurrent or metastatic HNC. The trial found that, for tumors with a PD-L1 score of 1 or greater, patients responded to single-agent pembrolizumab with superior overall survival compared to combination platinum, 5-FU, cetuximab (gold standard) regimens and had fewer adverse events. Another significant finding from the trial was that pembrolizumab plus platinum and 5-FU had better overall survival regardless of PD-L1 status compared to the combination platinum, 5-FU, cetuximab regimen. These findings lead to the FDA approval of pembrolizumab as a first-line agent in treating recurrent or metastatic HNC with a PD-L1 staining score of 1 or greater. For patients with a lower PD-L1 staining score, first-line pembrolizumab plus platinum and 5-FU is the new standard.
As a result of immune checkpoint inhibitors improving survival and reducing toxicity, their use in earlier stage disease, in combination with radiation therapy or other therapeutic agents, and deintensification have great potential. Our panel on Cancer Immunotherapy at the annual American Academy of Otolaryngology-Head and Neck Surgery meeting will provide an update from several ongoing trials and recent publications. A few of the topics you can expect covered are:
- A phase II trial of pembrolizumab + radiation for cisplatin-ineligible HNC showed toxicities comparable to those seen with radiation alone and very favorable one-year survival rates.
- For patients with high-risk HNC who can tolerate cisplatin, immune checkpoint blockade has been added to definitive chemoradiation regimens, with the intent of improving survival.
- One study added pembrolizumab to radiation and weekly cisplatin and found the combination was safe.
- Two large and randomized placebo-controlled studies adding anti-PD-1 or anti-PD-L1 therapy to cisplatin chemoradiation for patients with high-risk HNC are underway.
- Several clinical trials are investigating the use of checkpoint inhibitors alone or with other immunotherapies before surgical resection of HNC. The advantage of these models is that they allow for an improved understanding of responses and the biological impact of checkpoint inhibitors on tumors.
- Several phase II studies have used checkpoint inhibitors in the neoadjuvant (before definitive therapy) setting or combination with postoperative chemoradiation in HNC.
- A phase III study investing neoadjuvant and adjuvant pembrolizumab for patients with high-risk, resectable HNSCC (KEYNOTE-689) is underway.
Although we need to await the results of these clinical trials, likely, PD-1 checkpoint inhibitors will soon be integrated into a standard therapy for previously untreated, locally advanced HNC. Tune into our Cancer Immunotherapy panels to get an update on this exciting treatment modality for HNC.
Dr. Sweeney is employed by Louisiana State University Health and Science Center
Image by MOLEKUUL / GettyImages