Victor Ekuta is a 2020–2021 Doximity Research Review Fellow. Nothing in this article is intended nor implied to constitute professional medical advice or endorsement. The views expressed in this article are those of the author and do not necessarily reflect the views/position of Doximity.
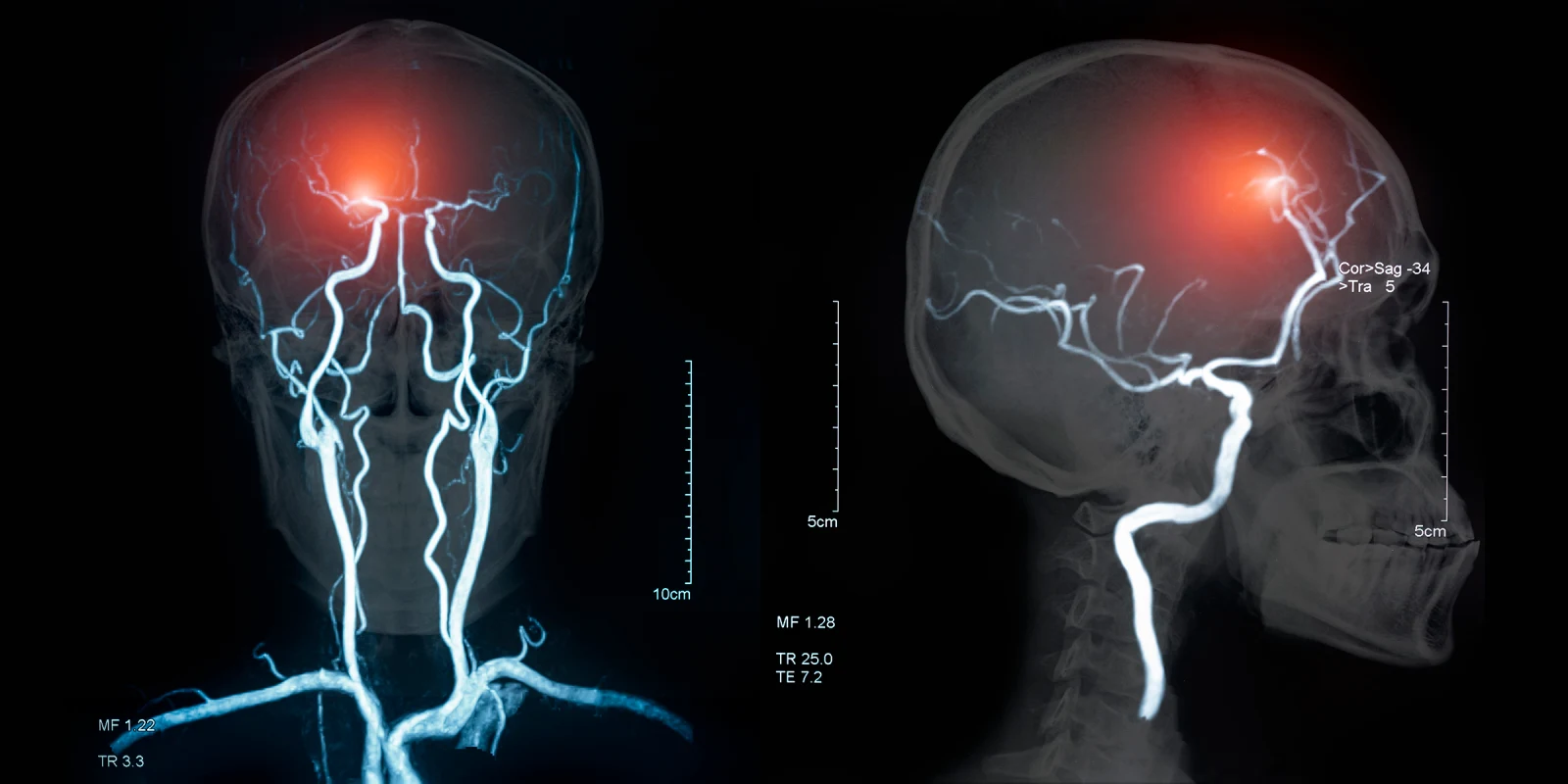
In a recent study published in The Lancet Psychiatry, Varathraj et al. shed light on the potential link between COVID-19 and neurological and psychiatric symptoms. The most common complications observed in the sample population were stroke (in 77 of 125 patients) and altered mental status (39 patients), but the study also revealed a striking association between symptoms and age, as 49% of patients with altered mental status were under age 60, whereas 82% of patients with cerebrovascular events were over age 60.
Though the study data is compelling, caution must be exercised in interpreting its results. To investigate the breadth of COVID-19 brain complications, the researchers set up a secure, U.K.-wide online network for specialists to report on the details of specific cases. This type of study design raises serious concerns about possible reporting bias, as the patient cases submitted for inclusion likely represent the most severe COVID-19 cases, as well as the most severe neurological and psychiatric manifestations. Similarly, focusing study inclusion on patient cases severe enough to require hospitalization raises questions about generalizability to the broader population of COVID-19 patients, most of whom are mildly affected or asymptomatic. Further, as the study was a descriptive, surveillance study lacking a control group (i.e., patients hospitalized with COVID-19 with no neurologic or psychiatric complications or patients experiencing neurologic or psychiatric complications without COVID-19), it challenging to ascertain the degree to which the observed neurologic and psychiatric complications are driven by the COVID-19 infection, versus other variables.
Varathraj et al. highlight a clear association between COVID-19 and neurological and psychiatric manifestations, but future research is needed to clarify the scope of these symptoms. Well-designed studies are needed to disentangle whether the neurological and psychiatric sequela of COVID-19 are due to direct viral invasion in the CNS, or reflect more widespread immune system activation, such as cytokine storm or antibody-mediated disease. Consideration should also be given to the fact that psychiatric manifestations may reflect pandemic-associated psychological distress, precipitated by uncertainty about the future, social distancing measures, financial losses, and fear of illness. Additional studies should also focus on understanding the underlying risk factors associated with the development of neurologic and psychiatric complications in individuals with COVID-19, and the incidence and prevalence of these conditions in the broader population of COVID-19 patients. Lastly, in this cohort, acute alterations in mental status were overrepresented in younger patients. The authors suggest that alterations in mental status are less likely to be attributed to delirium in younger patients, but additional studies should seek to clarify this relationship further.
Ultimately, this study underscores the importance of keeping COVID-19 on the differential when evaluating patients with new-onset neurological and psychiatric symptoms to avoid delayed COVID-19 diagnosis or misdiagnosis.
Victor Ekuta is an MD candidate at UC San Diego School of Medicine. He has previously served as a TEDMED Research Scholar and a Doris Duke Clinical Research Fellow, among many others. In the future, he plans to specialize in academic neurology as a physician-scientist-advocate, employing novel approaches to treat human brain disease, combat health disparities, and boost diversity in STEM.
Image by create jobs 51 / Shutterstock