Ever since the TV show of the same name came into existence, I have heard patients complain about procedures being “botched.” The show has normalized the concept of “surgery gone wrong,” and patients will routinely use the word to express their dissatisfaction with the aesthetic outcome of a surgical result, regardless of the health outcome. Every time I hear it, the word “botched” makes me cringe.
According to the dictionary definition, “botched” is used to describe “something, usually a job, that is done badly.” But in my experience, even surgeries that don’t look perfect are often done well. For instance, a patient may not have as “flat” of a stomach as she wanted after a successful liposuction. Or she may have experienced a known and treatable complication, such as a scar that may be wide or hypertrophic. In these situations, the result is still good, just not flawless. But for patients living in a social media-obsessed world, good is not good enough.
For surgeons, understanding the context in which our patients come to us is crucial. Like the rest of us, they are inundated by images of the most pristine results, amazing transformations, and instantaneous perfection via social media — without any insight into the long-term outcomes. Furthermore, online posters rarely share less-than-ideal surgical transformations — so patients’ assumption, as observers, is that no result is ever bad. No result is ever average. Every result is always perfect.
Cognizance of the misrepresentation and assumptions at play, as well as of our own personal insecurities, hopes, and dreams, can help clarify where our patients are coming from when they use the term “botched.” Regarding the latter element, we all know our own bodies well. It makes sense, then, that when we have surgery, the new scars seem to magnify every imperfection. And when the surgical results aren’t as we envisioned — e.g., one nipple that’s slightly higher than the other, or one breast that’s slightly larger — we may believe that our procedure, rather than our self-image, was “botched.”
Indeed, I’ve heard people say that “body dysmorphia keeps plastic surgeons in business.” While this may elicit a wry laugh, it’s also not entirely wrong. We (I say we, because I, too, have had multiple plastic surgical procedures) may have insecurities that lead us to seek out aesthetic surgery — for example, being ridiculed for being flat-chested, or for having breasts that are excessively large; or being self-conscious about excess skin from weight loss. When we seek out a plastic surgeon to help us address these issues, then, the experience is inevitably emotional and charged.
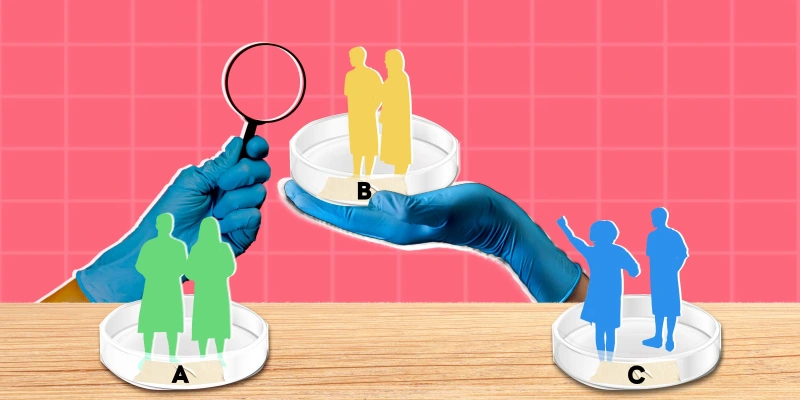
This complex interplay of external and internal factors leads us to the issue at the heart of the term “botched”: The tension between patients’ expectations and the reality of surgical outcomes, including complications. The task before us as medical professionals then, is to figure out: How can these two sides be reconciled?
As a surgeon, I know that surgery is unpredictable. Human beings are different. Sometimes there will be unforeseen issues. I recall being told by my attendings when I was a resident, “If you don’t have any complications, you aren’t operating enough.” I remind myself of this phrase every time I have an outcome that I’m not happy with — whether a complication or a dissatisfied patient.
What is the difference between a complication, a less than perfect aesthetic outcome, and a “botched” procedure? A complication is something that goes medically awry, such as an infection, or, say, the development of capsular contracture following a breast augmentation. Complications can beget suboptimal aesthetic outcomes — e.g., when the infection leads to an open wound, which leads to delayed healing, which leads to an ugly scar. Generally, however, a suboptimal aesthetic outcome refers to something more superficial: asymmetry between breasts, a widened scar, or a contour irregularity following liposuction — all of which may occur because the patient is human, as am I.
Statistically, we know that complications following surgery happen. They can happen when patients have a history of high risk behaviors, such as smoking, diabetes, obesity, etc. And they can happen when surgeons use poor judgment, such as when we excise too much skin on an abdominoplasty and create excessive tension on the closure, potentially resulting in a widened scar or worse, dehiscence.
Botched procedures, however, are not a part of the surgical vocabulary. Rather, we surgeons speak in terms of risks, outcomes, and expectations. The problem with the word “botched,” even when used colloquially, is that it implies that surgeons are incompetent, or worse, that we don’t care. Both are wrong. What’s really at stake is that the bar is set quite high: In other types of surgery, a “successful outcome” involves saving a patient’s life or removing a patient’s tumor, whereas in plastic surgery, not only does the patient have to do well surgically, but they also have to look well aesthetically. The surgeon-writer Atul Gawande has addressed the weight of these expectations in an interview: “In most medical writing, the doctor is either a hero or a villain. What I am trying to do is push beyond that and show how ordinary doctors are — and at the same time show that what they can do is extraordinary.” When we as people are less than perfect, in other words, it becomes difficult for us to produce a perfect aesthetic effect.
Realistically, we surgeons know that a poor outcome could happen to anyone. I recently treated a patient who had significant complications following a cosmetic procedure in another country. She had an infection of her breast implants, resulting in their removal and in the loss of one of her nipples due to necrosis. While this isn’t the ideal outcome, both of these are known complications of breast implantation. As my staff referred to her procedure as “botched,” I cringed — the implication was that we (my office and staff) are immune from the same complications, which is simply not the case. I myself have had patients who have had an infected breast implant. I would suspect if you spoke with most plastic surgeons, they would say that they have, too. I have also had patients with nipples that have been ischemic and that required intervention on my part. The fundamental difference in these situations is that I have been available for my patients. This patient traveled to a country where surgery was cheaper. Once she experienced these complications, her surgeon was no longer available to assist her with the management and treatment.
When a patient, any patient, says that her procedure is “botched” or that she doesn’t look as she had hoped, she doesn’t understand that what we hear is that a botched surgery means a careless surgery. And as surgeons, all we do is care. I for one review every procedure, every complication, every less than perfect result — I take them home with me, study the pictures, look over my operation notes, and read more articles. I think of what I can do differently next time. I think of how to make things better. I have spent countless hours in therapy trying to overcome the self-blame that arises when I have a less than perfect outcome. But my patients don’t see this side of me — rather they are disappointed at best, vindictive at worst. I am sympathetic, but I also know that in order to keep doing a good job as a surgeon, I have to practice both compassion and self-compassion.
But by now you may be wondering: Can a procedure ever really be “botched”? I suppose that yes, it can. My bar for a “botched” procedure, however, is much higher than my patients’. When they use this word with me, then, I try to do the following: Remember the forces that are working on them — and that I myself am not immune to, either. Educate them about the difference between perfect aesthetic outcomes, suboptimal aesthetic outcomes, and complications. Remind them that I know that plastic surgery can often be fraught — and that I’m on their side.
What colloquialism makes you cringe? Share in the comments below.
Dr. Anureet Bajaj is a plastic surgeon in private practice in Oklahoma City, Oklahoma. She enjoys running, painting, and spending time with her dogs and family. Her IG handle is @bajajplasticsurgery. Dr. Bajaj is a 2022–2023 Doximity Op-Med Fellow.
Image by user798987 / GettyImages