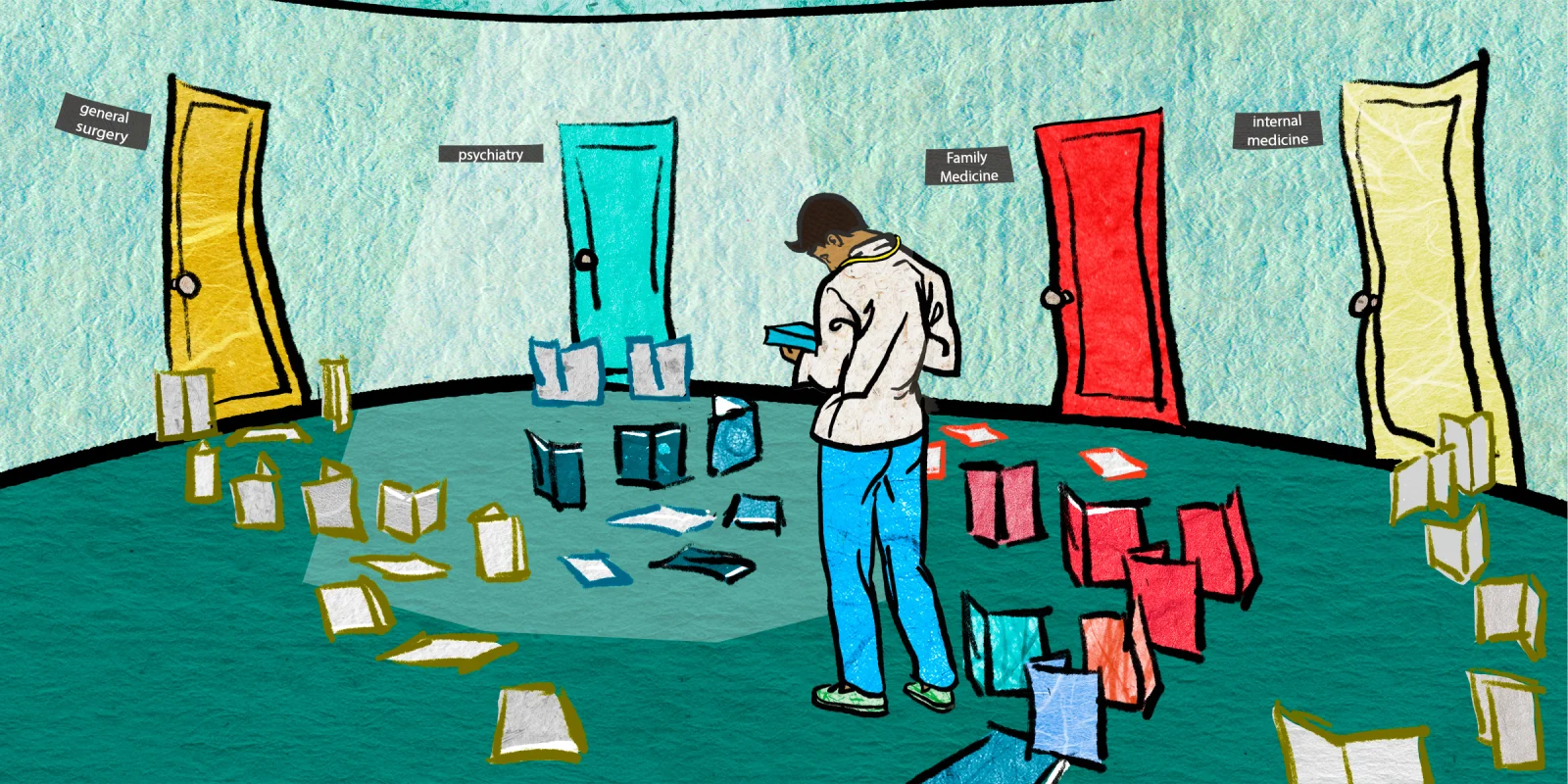
I regularly ask my colleagues how they chose their specific field and find the answers converge to a few common themes. Most of my peers answer that they had a rotation that they enjoyed during medical school or had already formed biases going into their clinical rotations that guided and informed their eventual selection. While this may seem like an acceptable methodology, I can’t help but wonder if the system is actually designed for individuals to make a truly informed decision. Do we even have enough information to choose our specialty?
Most medical school curricula are focused on “basic sciences” during the first two years, which is essentially a process of learning detailed histopathology at a level that is, practically speaking, irrelevant for clinical utility. In 10 years of practice, I have yet to identify a situation where a memorized regurgitation of the TCA cycle has offered value to patient care. The clinical relevance aside, this process of formal memorization occupies nearly half of our medical education. We then advance to clinicals where a mandatory base of “core rotations” is required for the majority of the subsequent 2 years, leaving us with three to four months in electives to decide our eventual careers. Moreover, select competitive specialties require research and advanced planning in order to build an application. Research activities are a formality for most candidates and, though a positive contribution to the field overall, take away precious time that can be otherwise carefully used to select a future career. Many students now outplay the game by picking research in the most competitive specialty in the first two years in order to get a leg up on the competition. While admirable strictly from a competitive drive, this Machiavellian instinct can simply validate overzealous decision-making based on ego as opposed to passion. One is encouraged to leap first and focus on building an application, rarely pausing to question whether they actually want said position.
While I recognize the value of a well-balanced education, this lack of emphasis on career selection seems absurd given the enormity of this decision. We end up wearing this choice for our entire careers. If our entire education consists of 48 months, why not use that time as effectively as possible for us to make our most informed choice? I can still recite (some of) the features of rare genetic syndromes but have never rotated through various surgical subspecialties, spotlighting another quixotic feature of the medical education system where we place impractical emphasis on identifying zebras. In today’s real practice, we can easily take pictures and look up facts on our phone in seconds – memory-based testing is a relic of the past. Instead, understanding fundamental principles of each specialty is more important than impressing teams on rounds with esoteric factoids. I also distinctly remember studying the nuances of biochemical pathways but never once had any formal instruction on ventilation settings or basics of trauma, which are true windows into the day to day work of intensivists and surgeons. Which topic seems more important to our eventual careers?
I realize there is an argument that I am ultimately responsible to seek out information in order to make the best choice for residency and I do think that position has some merit. Realistically, though, we are too busy focusing on the litany of exams and immediate hurdles to plan for the broader choice of residency. We aren’t encouraged to seek out mentors and evaluate our career priorities. We are rarely offered context about the lifestyle and financial considerations of each field or even the physical demands. For example, disciplines like interventional radiology, anesthesiology, and emergency medicine carry inherent stress and exhaustion that naturally cater to early retirement. This reality should be included as a disclaimer for anyone considering the specialty.
Status is yet another false driver of choice. Competitive individuals routinely seek out competition, and residency selection is not immune from this behavior pattern. I have seen many colleagues select a competitive specialty largely because of the prestige associated with the discipline. At many levels, I can relate as I enjoy a good challenge. However, I can’t help but wonder if some of my colleagues are actually matching their natural curiosity with their choices.
The system doesn’t really encourage us to make a careful choice; rather, we hurriedly pick something at the end of third year. At this point, we rely on a handful of rotations and reduce one of the most significant professional decisions of our career to a quick decision that is laden with incomplete information and biases. I know several colleagues that picked a specialty because they had an enjoyable time with a particular attending or a team of residents that happened to cross their path on a rotation. While this logic may seem relatable, it seems completely arbitrary. Many of my colleagues harbor a minor form of regret in their selection directly due to a lack of clinical exposure or incomplete information. They simply picked internal medicine because they knew what that field entailed and “liked it enough.” I fundamentally think the system fails us in this regard and places impractical weight on teaching material that will not be relevant for the lion’s share of our careers.
So, how to fix it? First, rewrite basic sciences to become clinically focused as opposed to molecularly-based and consider earlier exposure to all of the disciplines. Encourage students to make a truly informed decision on what their future careers entails by separating meaningful exposure from artificial hurdles (e.g., number of publications). Fundamentally, the emphasis of medical education should shift from a ritualistic memorization hazing to a sphere of education and awareness leading up to the most important selection of a burgeoning physician’s profession. As much respect as I have for tradition, the current tradition of haphazard residency selection needs to be re-evaluated. Moreover, I suspect we have too high of career mismatch — a resentful physician in emergency medicine may have been much better suited as an ophthalmologist but simply didn’t get the chance to rotate through that service. Though burnout is a multifaceted issue, I can’t help but wonder if maybe we wouldn’t burn out so quickly if we were more methodological in our career selection.
What did you learn about your specialty on rotations versus when you actually started practicing? Share a mismatch in the comments.
Dr. Chirag Parghi is a board certified radiologist with fellowship (subspecialty) training in Breast Imaging and is the proud Chief Medical Officer of Solis Mammography. His clinical interests are focused on the early detection of breast cancer. Dr. Parghi has been practicing radiology in the greater Houston area for 8 years, and obtained his MBA from University of Houston. He is a 2021–2022 Doximity Op-Med Fellow.
Illustration by Jennifer Bogartz