“Are you nervous?” I ask.
We’re sitting in the preoperative holding area. Just me, my patient ― a 20-year-old woman ― and her parents. It’s 7:15 a.m. They’ve been up since 4:00 — not from anxiety but because I’d asked them to arrive a few hours early to get a new MRI scan of her brain. I’ll put that updated scan into the OR's computer system, which I will soon rely upon to help me navigate safe passage to her tumor.
But who am I kidding? They’re terrified. It’s so clearly written on their faces. I’d have to be a robot not to notice the nervous laughter and her dad’s stale jokes ― a desperate attempt to lighten the mood and hide his own mounting panic. Hadn’t he always told her he’d keep her safe?
A few hours later, I finally reach the point in the operation that I always knew was coming. It has taken me a good hour just to expose the darn thing, working under the microscope dissecting a passable corridor above her cerebellum. The tumor, a benign but expanding rubber ball of cells the size of a chestnut, couldn’t have sprung up in a worse place: smack in the dead center of her brain. The central part, its core, has come out easily. Luckily, it was soft. But now I’m face to face with what’s left ― a bit of the capsule, which is stuck to the adjacent basal vein of Rosenthal, a thick blood vessel coursing along the back of the tumor remnant.
So here we are ― me, that last bit of tumor, and the vein, which I know is draining all the blood from her thalamus. If I accidentally damage this critical vessel then her thalamus — a cluster of neurons the size of a walnut — will probably swell up like a plum and she’ll never wake up.
I slow everything down: my breathing, my heartbeat, my thoughts. I focus my mind. I wedge the sides of my hands against the edge of her skull to make sure they are well braced to reduce any tremor. I block out any distractions, like a professional golfer standing over a 10-foot putt on 18, trying to ignore the crowd and the weight of the moment.
I start by teasing the tumor fragment. I nudge it to the left and then to the right, trying to see around back, where it’s attached. How stuck is it? Despite my gentle prodding, it won’t budge. I decide to try and cut it off. “Microscissors,” I say, as I reach out my right hand. The nurse replaces the coagulating tweezers I’m holding with a long delicate pair of pinching scissors.
We’re at maximum zoom on the scope — so deep that there’s barely enough light for me to see. The tips of my scissors are right there, but as far as I can tell, either I’m going to slice into the vein, which might create a gaping hole that I might not be able to close, or I’m cutting into the tumor, which risks leaving a piece behind.
I pause to consider: What’s my next move?
I wish I could say that this scenario is uncommon, but it’s not. This is where we brain surgeons — and most other surgeons, I imagine — find ourselves as a matter of course. We are forced to make decisions that will have a profound impact on another human being’s future. In one version of the story, they are cured and live a normal life. In another version, they are disabled or plagued by the relentless progression of the tumor I’ve failed to remove.
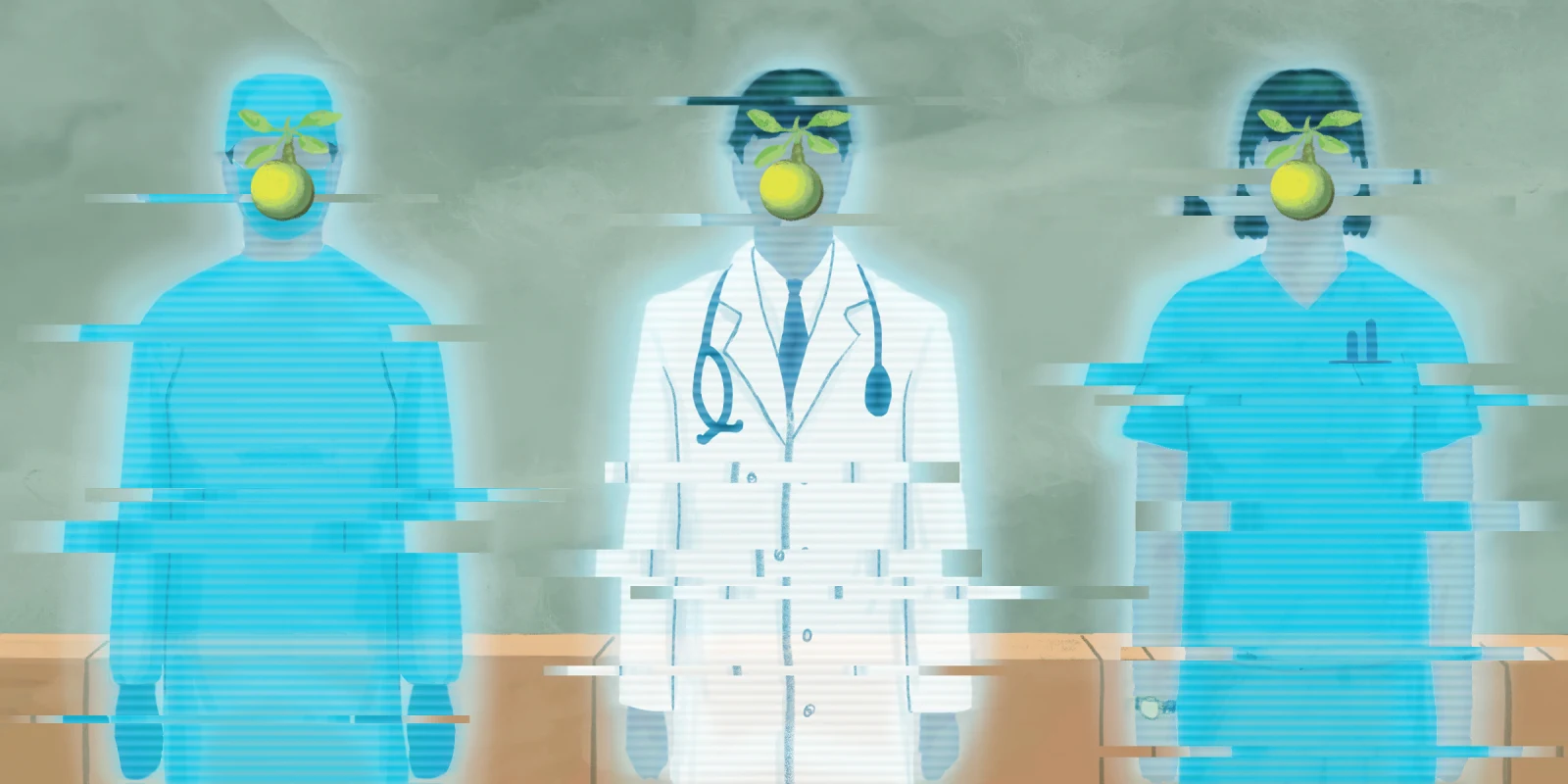
So how do brain surgeons make these types of decisions? That’s a question my colleagues and I have been asking ourselves as we consider the prospect of how artificial intelligence might change our craft. Could AI help us make better decisions than we might make on our own? Or, as some of my colleagues fear, could an artificially intelligent surgical robot replace us altogether?
Earlier this year, the first AI program specifically designed for neurosurgeons was released. Called AtlasGPT, it promises to help with preoperative decision-making, operative planning, and even surgeries. I’ve used the program myself. It’s quite impressive. Ask it a question about a clinical scenario you might encounter in your office, or in an ER, and it will spit out a list of treatment options derived directly from the thousands of articles, textbook chapters, and lectures fed into its memory banks.
If you ask it to outline the optimal surgical approach to remove a tumor buried deep in the brain, it will provide you with several options, describe your chances of success, and then expound on the risks of each alternative. It can even detail how to perform some of the most complex operations by providing a list of the key moves required to get the job done.
But is brain surgery like changing a tire? Can we reduce every physical task to a checklist? Airline pilots can manage most in-air problems by pulling out a manual, but can brain surgeons do the same? If surgeons do indeed make decisions based on rules, then surely an AI could do a better job than a surgeon by eliminating noise and bias. But if intuition, instinct, and creativity are paramount, then a digital doc might fall short of a real one.
As one of my professors used to remind me, “Surgery is a contact sport.” Performing surgery is not a “House, MD” quandary in which we sift through massive amounts of information stored in our memories to arrive at the best solution — the kind of thing computers do very well. It’s not like playing chess, or Go, or even diagnosing cancer from a mammogram. When it comes to surgical interventions, figuring out what to do is only the first step. The real challenge is in the doing.
During an average brain surgery, I make several hundred ― more like several thousand ― small decisions one after the other, each of which resembles a little physical puzzle, like the extrication of a Jenga block. Each move solves a different kinesthetic conundrum and must be conceived and executed to perfection lest the whole structure collapse.
Human beings are exceptionally good at solving physical puzzles. I would even argue that this is what the human brain was designed for. Think about it: Our brains evolved inside bodies whose sole purpose is to keep us alive long enough that we might have a chance to reproduce. Not only that, but we also evolved on an oftentimes inhospitable planet that dares us to prevail. We had to learn to evade predators. We were forced to design and build sturdy homes to shelter ourselves from the elements and natural disasters. We developed language so that we could work together with other human beings to grow food, hunt, and find water. We eventually learned how to identify, avoid, and then treat countless infectious diseases created by microscopic bacteria, viruses, and fungi — all of which are trying to invade our bodies to sabotage and reprogram our cellular machinery so that they, too, can reproduce.
Once we learned how to survive, our brains also needed to navigate a hierarchical social structure, attract a member of the opposite sex, copulate, and create a community to protect and raise our children so they could do it all over again. Basically, our brains were made to negotiate a hostile environment using our hands and symbolic language to help us cooperate with other people to stay alive and make babies.
Computers, on the other hand, were created inside metal boxes that sit on their designers’ desks. They were conceived to solve complex problems with numerous steps and quantities difficult for the human brain to grasp. Having been designed for this purpose, they are exceptionally good at it. In nine hours, the AI program AlphaZero taught itself to play chess well enough to become the greatest chess player this world has ever known. But computers are not good at solving physical puzzles because they lack physical intuition. They didn’t evolve in a constantly changing environment. They never had to figure out how to find energy or shelter or how to get along with other computers. It was all just provided for them. They remain in their Garden of Eden under the protection of their creators.
AIs evolved in a virtual ecosystem that adheres to very specific rules. If they’re playing chess, they can be sure that the size of the board is fixed and that the rook can only move in certain directions. The square playing field won’t randomly morph into a trapezoid and the rook won’t rashly decide to go rogue and leap diagonally over a few pawns to ambush the queen. As such, they are ill-equipped to enter an OR and face the fog of war with its unknown unknowns.
But there is also another, perhaps even more compelling, reason why brain surgeons may never be replaced by surgical robots, no matter how much more precise or steady their cybernetic limbs may be compared with my own.
Imagine you are riding in a self-driving car going 65 miles per hour down a winding road overlooking a cliff. Your life now depends on the perfect functioning of a machine that couldn’t care less whether it crashes. The guidance system behind the wheel won’t be terrified of spinning out of control, nor will its heart begin to race when it comes too close to the edge. It won’t necessarily slow down around the most treacherous corners because it has no skin in the game. While its mechanical precision might not be subject to the vicissitudes of performance anxiety, when it begins to malfunction, you won’t be able to reason with it or appeal to its sense of self-preservation, because there is no “it.”
Likewise, when you are unconscious and anesthetized on the OR table, a surgical robot will never make its decisions as if you were a member of its own family. It will not feel guilty if you wake up paralyzed at the end of the operation. It will never look you in the eye and promise to do its very best to make sure you leave the hospital intact. God forbid there’s a complication; nobody will be there to apologize to you, and there will be no one to blame, except yourself, for agreeing to let a heartless automaton do the job of a human being.
Brain surgery, or any surgery for that matter, is a deeply human endeavor. It leverages the strengths of our biological brains, which were designed to anticipate and solve material challenges in the physical world, as well as our sense of compassion, which compels us to take pity on a fellow human being in need and do everything in our power to restore them to good health.
Back in the OR with my 20-year-old patient, I am facing a decision. I think about what I would want done if this were my own daughter on the table. I have two girls about the same age. I think about their dreams, their expectations, and the lives ahead of them. I feel the tears well up as I imagine walking each of them down the aisle. I spend another few seconds staring at the vein and the tiny recalcitrant fleck of tumor. It’s benign after all. Sure, it might grow back in another 20 years. She might need to deal with it again someday, but she has an awful lot of living to do before that day arrives. “We’re closing,” I announce. I need to honor a father’s promise to keep his daughter safe.
Dr. Theodore H. Schwartz is a professor of neurosurgery at Weill Cornell Medicine in New York City and the author of the new book “Gray Matters: A Biography of Brain Surgery.” Previously published in The Boston Globe.
Illustration by Diana Connolly