Janice was 38 years old when she was diagnosed with a relatively rare brain cancer called Glioblastoma Multiforme or GBM. She presented to our ER after having a seizure at work. An MRI demonstrated a 3 centimeter ring-enhancing mass in her right frontal lobe. She was admitted to the hospital and taken to surgery two days later. Janice had an extensive craniotomy with excellent resection of the tumor on postoperative MRI. She recovered well and was discharged from the hospital. A few weeks later, she started temozolomide chemotherapy and intensity-modulated radiation therapy. She tolerated these treatments well.
Many months later, she started not feeling well. She was nauseous, vomiting, and fatigued. After her sixth cycle of chemotherapy, she took a pregnancy test. It was positive.
Janice had an appointment with her obstetrician and an ultrasound was done that placed her gestational age at about nine weeks, which meant that she had had two cycles of chemotherapy while pregnant. A second ultrasound about three weeks later by a maternal fetal medicine specialist revealed a very poorly developing brain and obvious limb atresia.
Janice and her husband had been married for about 13 years and already had one young child when she was diagnosed. During our clinic visits before and after surgery, I didn’t specifically ask them if they had plans for more children and as her neurosurgeon, it didn’t occur to me to discuss with them the risks of chemotherapy and radiation should she get pregnant. Even with that lapse in conversation, preoperatively, Janice took a pregnancy test and a second pregnancy test before she started her first cycle of chemotherapy and radiation. The cancer center directing her care didn’t discuss the risks of pregnancy during chemotherapy and radiation, and there was no version of a written consent that discussed pregnancy before treatments began. Janice had taken it upon herself to take three other pregnancy tests during sic months of chemotherapy. It was only after she finished her sixth cycle of temozolomide and a fourth pregnancy test that it came back positive. Janice and her husband said this pregnancy was unplanned and they were not trying to get pregnant. Now they are faced with the decision of stopping treatment for the duration of the pregnancy in a cancer that is almost uniformly fatal and survival is measured in weeks — most patients pass away two years after diagnosis.
How should we being to counsel this patient? Who should be counseling her?
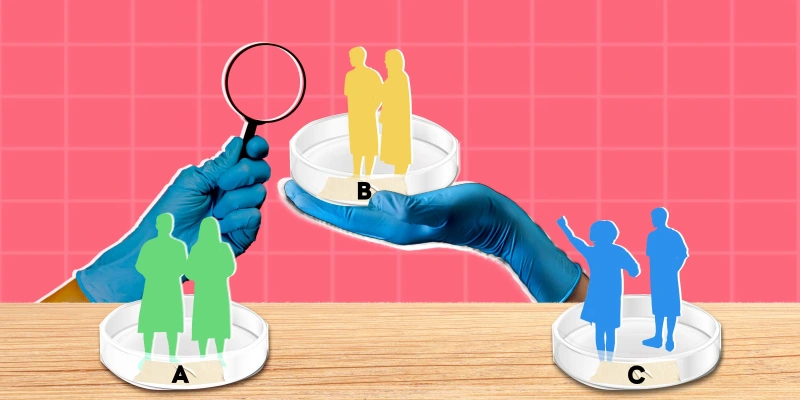
Shall we start with the topic of routine testing of patients of childbearing age diagnosed with cancer and undergoing chemotherapy? What about the concept of informed consent for a patient of childbearing age before chemotherapy is started? Should fertility preservation options such as egg harvesting and sperm banking be discussed after a diagnosis of cancer and part of an informed consent prior to chemotherapy?
Many comprehensive cancer centers make pregnancy testing a routine lab during chemotherapy. Many also have a detailed informed consent before chemotherapy that addresses the issue of pregnancy. The National Comprehensive Cancer Network recommends “pregnancy screening should be integrated into treatment pathway, clinical guidelines, and organizational policies, as well as into clinical workflows to avoid the unintentional treatment of a pregnant woman with cancer.”
What about the patient getting unexpectedly pregnant during chemotherapy? Should we have recommended the patient take more aggressive birth control precautions knowing that a fetus could be significantly affected by chemotherapy? Case reports of the use of temozolomide during pregnancy have appeared in the literature but data is limited. A risk of adverse events during pregnancy with the use of other chemotherapeutic alkylating agents has been established. Lifestyle changes in the setting of pregnancy to ensure a healthy fetus has been common practice for decades. For example, obstetricians have told their expectant mothers to quit smoking and cease alcohol consumption during pregnancy because of the known teratogenic risks.
Another layer is the type of cancer Janice has. Routine care of GBM patient involves MRI of the brain with gadolinium contrast every 10 to 12 weeks. However, under routine circumstances, the use of gadolinium contrast is not recommended in pregnant women. According to American College of Obstetrics and Gynecology guidelines, “The use of gadolinium contrast … may be used as a contrast agent in a pregnant woman only if it significantly improves diagnostic performance and is expected to improve fetal or maternal outcome.” Pregnancy in a GBM patient may limit the ability to properly monitor the patient’s tumor and detect an early recurrence.
Does Janice’s husband have any consideration in this process? The mother of this child is likely to die from her cancer diagnosis and there is a risk the child could be born with significant medical and developmental challenges. This is likely to leave the father as the sole caregiver in a difficult situation.
What is the physician’s obligation regarding treatment in this circumstance? Can the physician elect to not offer cancer treatment for this patient’s cancer in the setting of pregnancy because of concerns for the health of the fetus? As physicians, we withhold treatments all the time because of potential teratogenicity. Usually, these treatments are not life-threatening and risk is accepted with little discussion.
There is one more important factor to Janice’s story: She lives in a state that currently outlaws elective termination of pregnancy unless the life of the mother is in danger.
Let’s say for the sake of argument, the patient did want to pursue elective termination of pregnancy. As stated, in the state she lives in, she can terminate only if her life is in danger. Is her life in danger? The pregnancy itself isn’t threatening her life — but the cancer diagnosis is. So, if she withholds her cancer treatments, does that mean the pregnancy is threatening her life? And don’t forget we’re talking about a cancer that is almost uniformly fatal with or without treatment.
I never thought when I became a neurosurgeon that I would be putting this much thought into these issues. But it’s an excellent reminder to never forget that no matter how focused your practice is, no matter how specialized your particular niche in medicine may be, it is difficult to be a good, effective, caring physician without being aware of and taking care of the whole patient.
Dr. Gruber is a Neurosurgeon in Paducah, KY. His clinical interests include brain tumor management and robotic spine surgery. Find him on Twitter @DrThomasGruber and LinkedIn. Dr. Gruber is a 2022–2023 Doximity Op-Med Fellow.
All names and identifying information have been modified to protect patient privacy.
Illustration by Diana Connolly