School prepares us to be novices. The tricky part is that the type of people who are drawn to be NPs are often highly motivated overachievers; the thought of being a novice is hard to live with. Add to that the fact that becoming an NP comes after having gone through the novice stage as a RN, and it becomes an even harder pill to swallow.
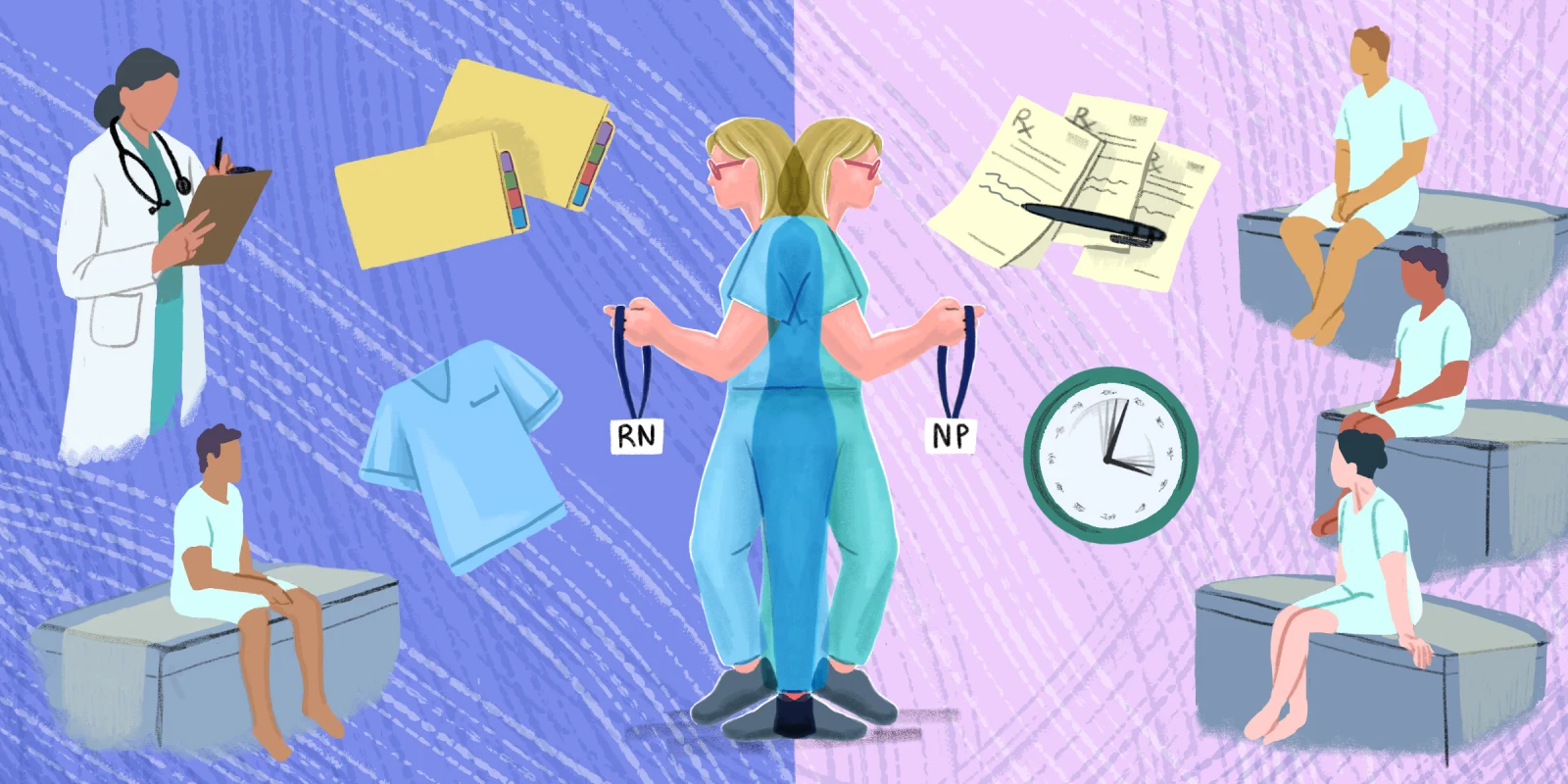
NPs are not simply RNs with more education. We are RNs who elected to advance our education and shift into a different role in the health care ecosystem. So why do so many of us struggle with this role transition? I believe it’s because we are taught the what and the why, but not the how of being an NP.
Nursing school gave me the what. It was there that I learned about working with patients directly. This made sense because the role of an RN, especially a new graduate, is often working directly with patients at the bedside. A lesson that sticks with me is the principle of referring to patients by name, even in giving reports — never simply by their bed number or diagnosis (“Mr. Smith” rather than “318 with the CABG”). The soft skills of role development were baked into my nursing program, and many other programs like it. But I left nursing school feeling I was missing depth in my education. I kept wondering if this was the semester that we were going to get that deeper understanding and knowledge of the topics that we were learning about. I was taught how to care for a patient with a certain diagnosis — for example, hypertension — but I didn’t get a nuanced understanding of why some people are more at risk than others, why an ACE inhibitor is the right choice for some patients and a beta blocker is better for others.
NP school gave me the why: why it mattered if your hypertensive patient also had a diagnosis of asthma, why hypertension tends to affect people as they age (but not all people, and not the same way), why lifestyle factors are the first move we make for many patients with hypertension. In NP school, I got to pull back the curtain of clinical knowledge and see more of what was happening behind the scenes.
And then there’s the how. When we cross the academic finish line as NPs, many of us are shocked by the amount of non-clinical/role transition work left to do (and left for us to do without much of a guide). We are out here on our own, and find out that we got the what in nursing school, and the why in graduate school, but no one really clued us in to the how. We know that we are now responsible for diagnosing and treating our patients, and have a better understanding of the nuanced pathophysiology, but how we navigate our new roles often remains a mystery.
How do we balance our time with our patients with the sharply increased amount of paperwork that waits for us? How do we navigate this new role as the place where the buck stops? How do RVUs work? How do we deal with impostor syndrome? How do we balance the new pace and hours of being an NP, compared to an RN? Sometimes we get examples of what to do (or not do) through our clinical rotations, personal experience, or maybe at our previous jobs. But curriculum-based learning focused on the role transition, meshed with the broad clinical base that we are learning in graduate school? Rare, at best. Most of the learning that we do on this subject is through trial and error, instead of role modeling or training.
How do we address this? I’ve got some ideas. Our graduate education should guide not only the development of our clinical knowledge, but also our professional role change. An NP is not simply an RN with more education, and our curriculum needs to reflect that.
The clinical rotation setting is another opportunity for nurturing this change. Practicing the guided application of clinical knowledge should always remain the foundation of the clinical rotation, but addressing the ways that we approach these scenarios in our new role is necessary and helpful to emerging NPs. Failing to do so sends new NPs into practice with a hurdle.
Residency programs may be the ideal solution to this role transition from RN to NP, but accessibility is a major barrier for many. The reasons for this are multiple: the need for relocation, reduced salary, competitiveness for a small number of openings. Many NPs have families and roots in their community, so relocating for a one-year residency is out of reach. Reduced salary is another barrier; the promise of increased earning is a draw for many NPs, and a reduced salary (even for a year) is a tough sell. NPs often compare their salary to “what (they) could make” as an RN (never mind the fact that the two positions are very different). The thought of having a salary that is $10,000-$20,000 below what their peers are making is a tough sell.
If residency programs were included in academic programs, lengthening them by 6-12 months, this might address some of these barriers. This would produce increasingly confident new grad NPs who emerge with much of the role transition already addressed. Offering residency programs in an online/remote format would eliminate the geographical/relocation barrier, while also taking concrete steps to address burnout before it starts.
The current model of jumping into practice immediately after graduation works for some, but comes with added struggle for most. Trying to find our rhythm while also adjusting to new work environments and new professional roles is a steep climb. Taking steps to ease the transition from RN to NP benefits not only the clinician, but the employer, the colleagues, the patients, and our profession.
How would you improve NP training? Share in the comments.
Jessica Reeves is a nurse practitioner as interested in the well-being of her fellow clinicians as that of her patients — and she's on a mission to make the work world a better place to live. She writes, works, and lives in the town that holds the world record for most lit jack-o-lanterns (really). Follow her at jessicareeves.net. Jessica is a 2023–2024 Doximity Op-Med Fellow.
Illustration by Diana Connolly