“Am I going to lose my arm, Doc?” This was the third time, unprompted, the patient had asked me this during a new patient visit to the orthopaedic oncology clinic. The patient — a woman in her early 50s with a three-month history of right shoulder pain — was referred from a local community hospital to my institution’s cancer center with a two-view humerus radiograph and CT scan demonstrating a complex appearing lytic lesion in the proximal humerus — metastatic disease until proven otherwise. Oftentimes, as is very reasonable, when imaging at an outside institution shows concerns for a possible malignant lesion, the rest of the imaging and lab testing gets deferred to the multispecialty team at our tertiary referral center.
With insufficient information to put a name to the disease, it would not be possible for at least another few days to determine what treatment options would be available. In our clinic, we usually try to avoid discussing treatment pathways until we have the full clinical picture, but it was obvious that this patient was hyperfocused on the thought of losing their limb, so I decided to pull at that thread a bit more. She then recalled, in vivid detail, her visit to the ER wherein the doctor that ordered the CT scan walked into the room, turned down the lights, and informed the patient with a very grave look on his face that she “had cancer and would probably need an amputation.”
Did this patient’s story have a bit of hyperbole? Perhaps. I will never know for sure how that ED visit went, but I know that, whatever happened, the patient walked away filled with a significant anxiety she would carry with her until her appointment in our clinic. However, these types of stories are not uncommon in our clinic. There are many avenues in which patients can obtain an anxiety-inducing diagnosis. I’m reminded of the woman that accompanied her septuagenarian dad to the clinic with a stack of information on “rhabdomyosarcoma” because a radiology report stated, unquestionably, this was what the patient had in his thigh. The patient did end up having a sarcoma but a histotype much more prevalent in his age group and one associated with a more favorable prognosis.
Similarly, almost weekly, we see a patient diagnosed with “liposarcoma” who comes to the clinic prepped for the worst because an online search led them down a scary path because they missed the preceding “well-differentiated” in the radiologist’s or pathologist’s report. For reasons such as this, there has been a push in my field to rename “well-differentiated liposarcoma” to “atypical lipomatous tumor.” Similarly, the World Health Organization has adopted “atypical cartilaginous tumor” to replace “low grade chondrosarcoma” in some anatomic regions. These sorts of name changes are not exclusive to musculoskeletal oncology, because … words matter.
At just past the halfway point in my musculoskeletal oncology fellowship, these types of interactions lead me to wonder, “Who is the best person to tell a patient they have cancer?” As one could imagine, a topic of this magnitude can be nuanced and require multiple conversations. However, putting a specific name to the disease opens up a Pandora’s box full of questions about prognosis and treatment options — a conversation that someone who doesn’t specialize in oncology may not be equipped to handle.
We actually have this sort of conversation frequently in our clinic because, even as specialists at a tertiary referral center, we don’t always have the answers immediately. The same goes for the other two oncology tertiary referral centers I’ve rotated at as a resident. I think, as clinicians, we often feel compelled to always have the answers to questions our patients may ask. In fact, I’d say one of the most difficult parts of joining the field of oncology has been informing patients that more testing is needed and navigating the uncertainty that comes with that statement.
In a few short years, I have seen a chronic expanding hematoma present like a sarcoma and an undifferentiated pleomorphic sarcoma present like a chronic expanding hematoma. I’ve seen a patient with surveillance imaging concerning for metastatic disease to the lungs end up having tuberculosis. And who can forget gout? “The Great Mimicker” is a moniker imprinted on me by the musculoskeletal radiologists on our Memorial Sloan Kettering Tumor Conference and Sarcoma Board. I’ve witnessed gout present in numerous different, very concerning ways.
So, with the complexities involved in reaching a definitive diagnosis and the nuances involved in treatment discussions, how do we approach these conversations? For starters, like all National Cancer Institute cancer centers, we have a weekly tumor board to discuss new and existing patients that present to various clinics at our institution the week prior. When malignancy, recurrence, or metastasis is a concern, we often have a discussion regarding who on the multispecialty team should be designated to inform the patient. The clinician chosen is based on numerous factors, including who is seeing the patient in clinic next, which team is most involved in the next stage of treatment, or whomever has established the best rapport with the patient to date.
That said, for clinicians who don’t treat malignant conditions as part of their daily practice, it’s probably advisable to refrain from having this conversation altogether. That is not to advise, by any means, to not make the patient aware of a concerning imaging or lab finding. In my opinion, it can even be appropriate to state something like, “this could be cancer, we are going to refer you.” It is OK to stop here and avoid potentially planting the seed of an incorrect diagnosis.
At this point you may be wondering what happened to the patient with the proximal humerus lesions. It’s worth noting that amputations for neoplasms are increasingly less common with advances in systemic treatments, radiation therapy, implants, and surgical techniques. Well, this patient underwent advanced imaging and a biopsy that ultimately demonstrated a solitary plasmacytoma of bone. The hope and expectation being treatment with no surgical intervention at all — a far cry from the amputation she was told she would need.
Who do you think should give a patient a cancer diagnosis? Share in the comments.
Kyle Walker, MD, MBA, is an orthopaedic surgeon who is currently training as the Sarcoma Advanced Research and Clinical Fellowship at U.C. Davis in Sacramento. He enjoys skiing, tennis, and spending time at the pool with his wife and two sons. He can be found on instagram at @kywalkermd. Dr. Walker is a 2023–2024 Doximity Op-Med Fellow.
*Certain aspects of some or all patients discussed above were changed in order to protect patient anonymity.
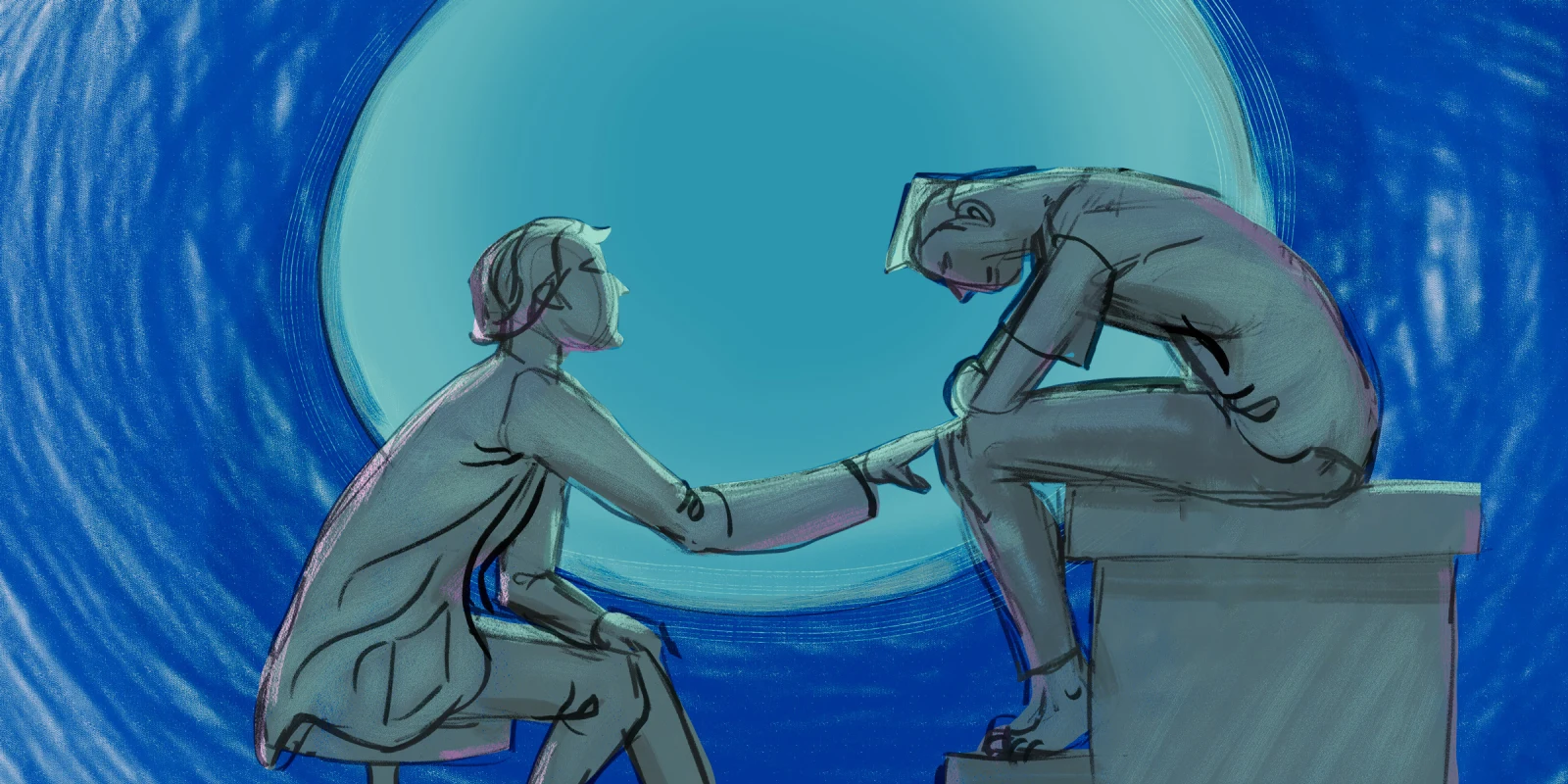
Illustration by Jennifer Bogartz