Abundance in health care sounds like a good thing, doesn’t it? We have tools and we want to use them. After all, when something is FDA-approved, it is like having multiple brands of an item on a shelf at a store, and we should be able to “pick” what we want to use given our training and expertise. But do we really get to choose, or is someone else out there choosing for us? And does that entity that is making these choices have the patient’s outcome in mind? The answer is no, not specifically. And certainly not in any sense of urgency.
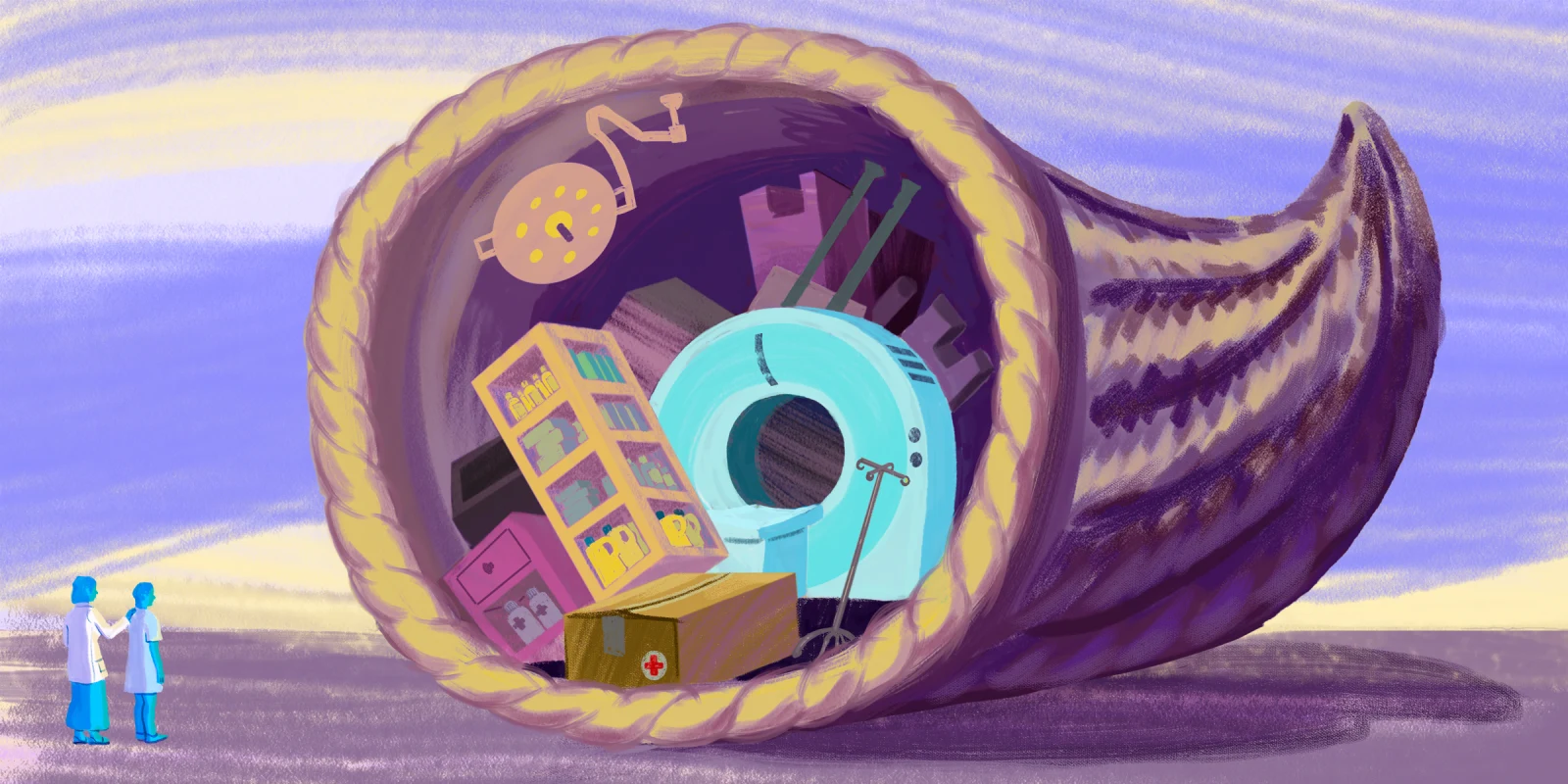
As physicians, we now have a treasure trove of medications, imaging modalities, and procedures at our disposal — all capable of improving outcomes for our patients. Biologics revolutionize treatment for inflammatory diseases, advanced imaging redefines diagnostic capabilities, and procedures in specialties like cardiology can prevent catastrophic events. Yet, paradoxically, this very abundance often keeps patients from getting timely care. This is not new news, but it is becoming more of a concern as we understand more about the diseases we are trying to treat. Poor health care creates poor outcomes. And the longer we wait to treat a patient’s condition, the more they are likely to have even more expensive complications, which then drives up the cost of health care even further.
Why? Because we have created systems where access to these life-changing tools is gated by unnecessary obstacles and by companies that are establishing roadblocks so that patients become someone else’s expense. Patients and their physicians are forced to jump through hoops, try inferior therapies, and endure redundant, low-value tests — all in the name of cost control or (outdated) policy. The result? Delays in care, worsening disease, and higher health care costs in the long run. Not to mention, more frustration, burnout, and lack of trust in the health care economy overall from both the patient and health care teams.
As a practicing rheumatologist, I see this phenomenon play out daily. But this issue is far-reaching and impacts every corner of medicine.
The Biologic Bottleneck in Rheumatology
The management of inflammatory arthritis, such as rheumatoid arthritis or psoriatic arthritis (PsA), has been revolutionized by biologics. These targeted therapies have given us the ability to reduce inflammation, protect joints from irreversible damage, and provide relief for patients whose lives were once defined by pain and disability. The science is clear: Early and appropriate treatment with the right medication alters the course of disease and improves outcomes. We have known this for decades now and the latest data suggests that patients who achieve low disease activity earlier in the course of their diagnosis have less comorbidities that affect other organ systems and have better health overall.
Yet, when I prescribe a biologic for a patient with PsA, the response from insurance companies is predictable. First, I am asked to prove that the patient has “failed” conventional DMARDs like methotrexate. Never mind that the evidence shows certain biologics work better than methotrexate as monotherapy for PsA. Never mind that the patient may have contraindications to methotrexate or that the drug might not address the patient’s unique disease phenotype. Never mind that my documentation states all these things and the bot that read my note did not actually record my clinical expertise as a reason to approve my prescription.
And if the patient has already tried one biologic? Insurance companies may mandate they switch to a “preferred” alternative rather than the medication I, the physician, deem best. These lists are impossible to find and are even more impossible to circumvent because each patient’s insurance plan is different from the last when it comes to covered medications determined by employers and insurance middlemen. These barriers create delays measured in weeks to months in the form of appeals and excessive paperwork to document what is already recorded in the patient’s medical record. During that time, my patients’ joints may sustain permanent damage. Their disease — a fire that requires prompt extinguishing — is allowed to smolder unchecked.
The frustration here is profound. The cost of early, appropriate treatment pales in comparison to the costs of joint replacements, disability, additional referrals, and lifelong pain management. Why, then, are we still forcing patients onto pathways we know by science are inferior?
When Superior Imaging Is Denied: Gout and Sacroiliitis
The delays are not limited to medications. Advanced imaging tools, which provide critical diagnostic clarity, often face the same uphill battle.
Take dual-energy CT scans in the diagnosis of gout. Gout is often misdiagnosed or underdiagnosed, leading to years of uncontrolled disease, recurrent flares, and permanent joint damage. Dual-energy CT is a highly sensitive and specific tool for identifying urate crystals and can confirm the diagnosis when a joint aspiration is inconclusive or impractical. Yet, these scans are routinely denied by insurance companies, forcing us to rely on plain X-rays, which often miss this disease entirely.
A similar scenario plays out in patients with ankylosing spondylitis (AS). For these patients, an MRI of the sacroiliac joints can identify active inflammation (sacroiliitis) long before structural changes appear on plain X-rays. Early diagnosis means earlier treatment with biologics that can stop disease progression. However, insurance companies often insist on X-rays first. And if the X-ray is “normal” — as it often is in early disease — patients are often told they don’t have AS and sent home to suffer for months or years until the disease becomes glaringly obvious.
The irony is striking: The very imaging tools that could prevent delays and improve outcomes are withheld, prolonging the diagnostic odyssey and worsening patient suffering.
The Electrophysiology Example: Unnecessary Hurdles in Cardiology
This isn’t just a rheumatology problem. In electrophysiology, procedures that could save lives or prevent hospitalizations are often stalled by layers of prior authorizations and stepwise policies.
Imagine a patient with symptomatic AFib. Catheter ablation has been shown to improve quality of life, reduce symptoms, and, in many cases, decrease long-term risks like stroke. Yet, before an ablation is approved, patients may be required to “fail” multiple antiarrhythmic drugs — despite the fact that these medications carry risks, are difficult to tolerate, especially for elderly patients, and are often less effective than ablation.
The delays are costly, both for the patient’s health and for the health care system. Uncontrolled AFib can lead to repeated ER visits, hospitalizations, and complications that could have been avoided. Just as in rheumatology, early intervention with the most effective tool is more cost-effective in the long run than a “wait and see” approach.
Abundance Should Accelerate Care — Not Delay It
The abundance of options we have in health care today is a gift. Biologics, advanced imaging, and sophisticated procedures represent decades of scientific progress. But this abundance should accelerate care, not delay it. These options should empower physicians to choose the most effective, evidence-based treatment for each patient, not trap them in a maze of step therapy, prior authorizations, and redundant testing.
To fix this, we need to shift our mindset:
1) Trust physicians to make the right decisions for their patients. We are trained to weigh risks, benefits, and costs. The current system, which prioritizes cost containment over clinical judgment, harms patients and erodes trust. Why do we rely on outdated practices to try to save a few dollars when the delayed outcome will cost significantly more?
2) Acknowledge the cost of delays. The downstream costs of untreated disease — hospitalizations, surgeries, disability — far exceed the cost of early, appropriate intervention. Treating a complex disease promptly isn’t just compassionate; it’s fiscally responsible.
3) Eliminate barriers to proven therapies and diagnostics. If the science supports a treatment or imaging modality, physicians and patients shouldn’t have to fight to access it. Policies like step therapy and imaging requirements need to be revisited through the lens of patient outcomes.
The Urgency of Now
As physicians, we see the urgency of treating complex diseases every day. For the patient with psoriatic arthritis whose joints are at risk, for the patient with ankylosing spondylitis desperate for a diagnosis, for the patient with AFib hoping to avoid a stroke — time matters.
Our health care system must recognize that delaying care to save money in the short term only leads to greater costs and suffering in the long term. Abundance should be a beacon of hope, not a bureaucratic burden. And why do we not have more health care economists reporting these figures and looking at outcomes rather than data at the moment?
It’s time to let physicians practice medicine and put patients first. It is also time to collaborate and study how our tools help our patients. Our tools are ready. Now, we just need the system to get out of the way.
Dr. Brittany Panico is a rheumatologist in Phoenix, AZ. She is a wife and mother of three awesome boys and enjoys hiking, being outdoors, traveling, and reading. She posts on @AZRheumDoc on Instagram and Brittany Panico, DO, on LinkedIn. Dr. Panico was a 2023–2024 Doximity Op-Med Fellow and continues as a 2024–2025 Doximity Op-Med Fellow.
Illustration by Jennifer Bogartz