My patient wanted to “do everything.” To her, this meant flying to Arizona and paying out-of-pocket for IV vitamin C.
Her cancer was rare, and the chemotherapy I had to offer was based on small research studies. So when she asked me about it, was it really so far a leap to try alternative therapies instead? But I tried to caution her on the difference between limited science and pseudoscience.
But I chose my words with care because I remembered the time, years previous, when I hadn’t. I was not long out of fellowship, and a patient had brought in some printouts from the internet. I’d thought I was doing the right thing, explaining about randomization to limit the placebo effect and the careful design of phase 3 clinical trials to validate efficacy. I still remember the words I used, although they make me cringe now. Not because there was anything wrong with their content, but rather the delivery — unintentionally sanctimonious: “We only use therapies that have been reported in peer-reviewed papers published in respected medical journals.”
I don’t remember what that patient said in reply, but I remember what he did. He stormed out of my clinic and never came back. I remember the anger and hurt on his face. I remember the realization that I’d gone about that very, very wrong. Since then, I’ve learned the most significant factor in my ability to communicate information to my patients comes down to one thing — whether they trust me.
Now, with my current patient, I didn’t admonish her. I tried to tease out how much it would cost her and what she hoped to gain from it. I told her that it wasn’t my medical recommendation. But she and I both knew that I couldn’t offer her a cure. All I could offer her was my promise that I would be there for her whenever she wanted to try the standard chemotherapy.
At her follow-up visit, a month or so later, she told me how great the vitamin C had worked. So well, in fact, that the tumor had eroded through her skin.
I examined her and tried to keep my face expressionless as I moved the gown aside. There lay the fungating tumor, where previously there had only been a palpable mass beneath the surface of the skin.
She kept talking throughout the exam. “They told me it would happen. That it would be a sign of the vitamin C working. Pushing the tumor out. Isn’t that wonderful?”
I thought hard about what to say. I thought about what kind of people would tell this to a patient. People who knew enough about cancer’s clinical progression to have known the tumor was close to erupting through the surface before they “treated” her.
As an oncologist, I know those signs all too well. First, erythema over the surface of the mass. Then the skin becomes taut and shiny. Next, an increase in nodularity. Until finally, the tumor breaks through.
It’s never a good thing. It’s the farthest thing from wonderful I could imagine.
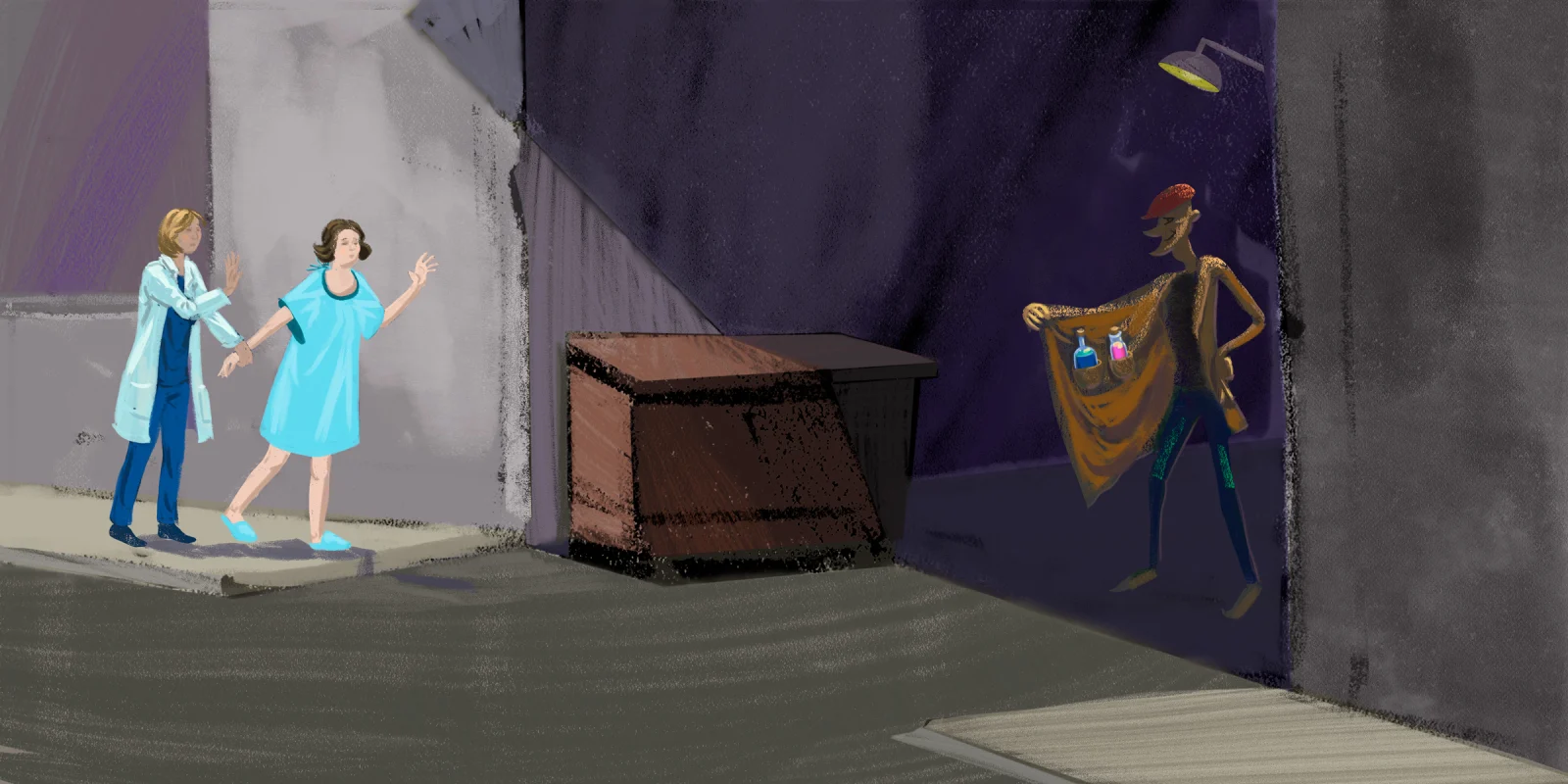
Clearly, the people offering the vitamin C knew these signs. But instead of sending her back to her oncologist, they continued to take her money. I tried to quiet my anger as I wondered: at what point does misinformation cross the line to harmful intent?
I sat down and explained this to my patient and her husband. That the tumor bursting out of the skin was a sign of disease progression and not a response to the vitamin C. No matter what she’d been told.
The next day, she decided to start the chemotherapy.
Years later, I find myself thinking of her now in this time when, perhaps like no other in the past century, people are being drawn to charlatans. What is it in our human nature that drives us to collectively eschew the experts and scientists and instead embrace internet celebrities and "snake oil" therapies? It’s nothing new; the word "charlatan" to signify a seller of dubious medical therapies has been around since the 17th century.
I know it’s a complicated matter, and I’m not suggesting I have the answers. But I think it might have something to do with this: The most dangerous lies are those that use the truth to sell themselves.
And a corollary: Sometimes, the most ignored truths are those couched in academic language and smugness.
Fifteen years after my mistake with that first patient, I’ve learned not to dismiss or belittle my patients’ ideas about their treatment. If they bring in information that they’ve printed off the internet, I look it over for them. And then I give them my opinion of it and explain why. But I don’t lecture them about peer-reviewed publications and medical journals. I speak to them from my heart.
And 15 years as a practicing oncologist has also shown me that even if they don’t want to believe me, in the end, cancer will reveal itself to be cancer.
What strategies do you use to talk to patients about alternative therapies? Share your stories of any patients who have had similar experiences with alternative therapies.
Jennifer Lycette, MD, is a medical oncologist in rural community practice on the North Oregon Coast. Her perspective essays have been published in NEJM, JAMA, JCO and more. Dr. Lycette was a 2018–2019 Doximity Author, a 2019–2020 Doximity Op-Med Fellow, and continues as a 2020–2021 Doximity Op-Med Fellow. You can find more of her writing at on her website, and follow her on Twitter @JL_Lycette. Opinions are her own.
All names and identifying information have been modified to protect patient privacy.
Illustration by Jennifer Bogartz