I was almost at the local Humane Society facility. While approaching a red light in my car, something in the rearview mirror caught my eye: A car had suddenly stopped some 50 feet behind me. But the driver was nowhere to be seen. As time passed, no one appeared in the car, and so I feared the worst.
As a second-year medical student, I thought about my role in this kind of situation. I had constantly been told throughout the year that, in my patient and standardized patient encounters, I was “only” a medical student, not a physician. I was no expert, no practicing clinician. Nonetheless, I turned my car around and headed toward the scene.
The rest of the situation happened as if another person had taken over my body, my true self detached from the event. I found myself with an ice scraper in my hands, slamming it against the car’s rear window. A man that had arrived helped me finish the job. I was then surveying a pulseless woman, slumped at the wheel. Could I trust myself enough to know whether this woman was in need of compressions? I somehow lifted her limp body into the left turn lane, with the phrase “Is the scene safe?” echoing in my head. I also continuously thought about the biggest factor in this woman’s potential survival: the time to the start of compressions. I laid out my winter coat on the road, then rolled her body onto it.
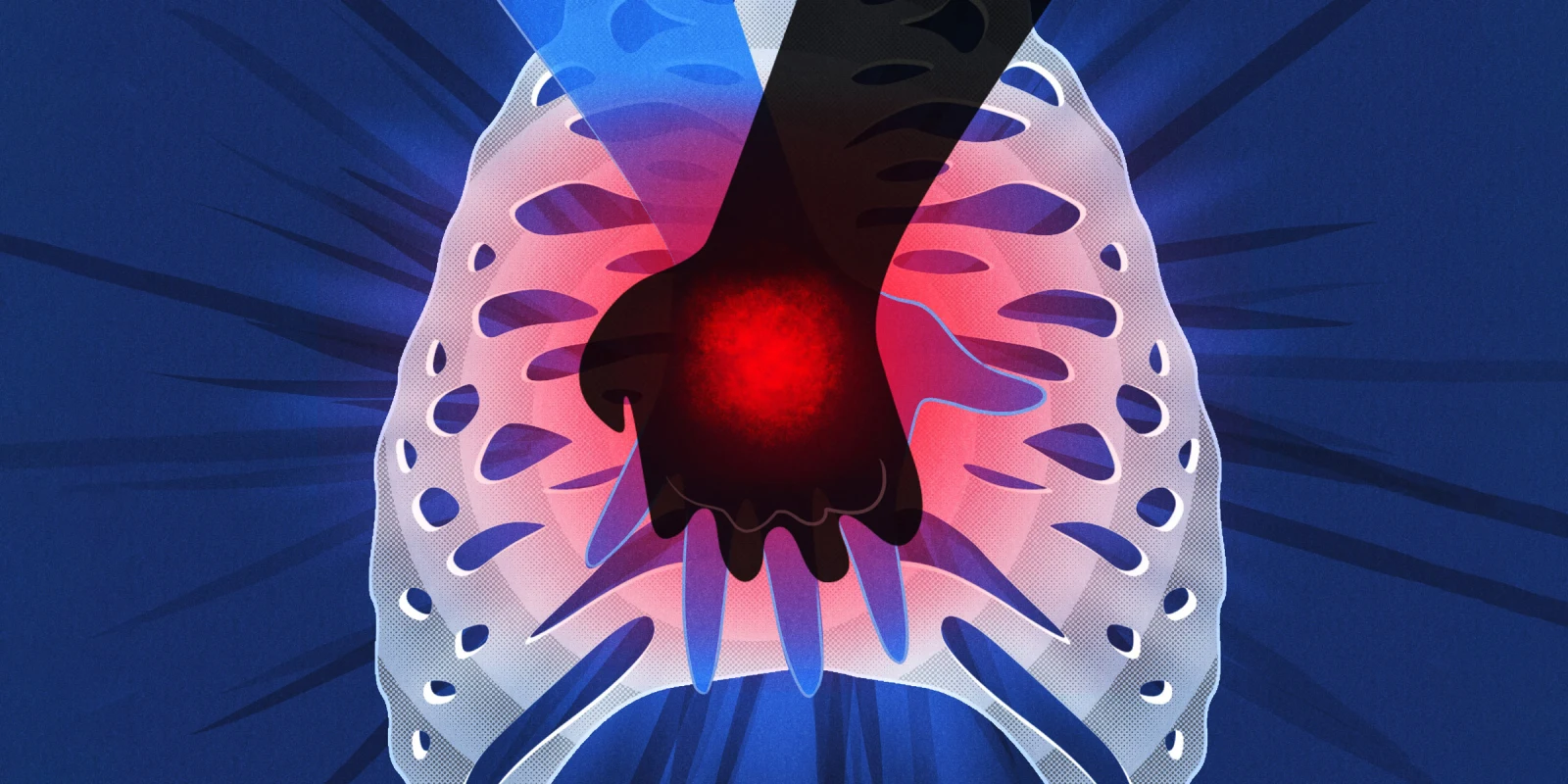
An audience gathered. With no one professing to know CPR or to help guide my clinical reasoning, I crossed my hands and pressed them onto her sternum. As I pushed down, the sound of her cartilage separating from her sternum traveled from my fingertips to my spine, reverberating in my ears. The lyrics “ah, ah, ah, ah stayin’ alive, stayin’ alive” moved across my lips as I compressed.
I found myself begging the woman to breathe — to live. She responded with an ineffective gasp, giving me some hope, yet she remained unresponsive. EMS eventually arrived and took over compressions shortly thereafter, scooping her up into the ambulance. I floated toward my car parked just a few feet away from my makeshift trauma bay. Soon after I drove away, I parked to decompress, and my true self returned to my body, and I began to cry.
I then did what anyone would do: I called my mom. When I was finally able to recount my story, I only felt worse. All of the things I did wrong ran through my head, and the doubts echoed constantly: I should have taken the time to get her to a safer scene. I should have done a precordial thump to give her a better chance at response. My mother, as always, was the emotional support I needed, but she had never had to compete against death in that way.
The memory of my drive home was a blur. I had my phone in my hand searching for Dr. Pedell’s contact on my phone. He had guided me through cases to present to my internal medicine interest group and taught me how to do a thorough review of systems, both the physical exam and the infamous social and sexual history — collectively, my medical foundation.
When he answered, I was able to recount the story, with many breaks in between words because of my tears. Why did the woman not revive? I had felt so close to helping her get there when she gasped for air.
Dr. Pedell’s response, in his words: When Nikki called with pain in her voice, I listened to her story and knew the breathing pattern she recalled. I gently explained agonal respirations, all the time leading up to informing her that this woman had most likely had a life-ending event and associated cerebral hypoxia. Nikki was, understandably, quite saddened. For the first time, someone had died literally in her hands. All I could think to do to improve her spirits was share similar memories I had in my career. We talked about PTSD-type symptoms she could expect to experience and told her my line was always open — that was all I could do.
After the event, I started to see the woman’s face during menial tasks. Dr. Pedell had warned me this would happen. I kept thinking back to what I had asked him on the phone: How long will it take to stop feeling like this after a patient dies in my care? His answer was he hoped I’d always have those feelings and use them to inspire future patient care. I imagine I won’t be initiating CPR on many of my patients as a child psychiatrist. I have heard, though, that as a psychiatrist it is not a matter of if one of your patients will die under your care, but when.
In response to this event, I thought that I might not be cut out to be a doctor, not strong or hard enough to endure the inevitable passing of future patients. Dr. Pedell was able to reassure me that my emotional response was not a weakness, but a quality of a good future physician with compassion for a patient’s fight. With the guidance of an empathetic mentor, I was able to reframe an experience that initially deterred me from continuing medicine into one that encouraged me to move forward and aspire to feel those feelings for the benefit of my future patients.
What motivates you to keep on amid the challenges of medicine? Share your experiences in the comment section.
Nikki Haggerty is in the class of 2023 at Oakland University William Beaumont School of Medicine.
Leon Pedell, MD, is a retired internist who taught physical diagnosis for over 40 years.
Illustration by April Brust