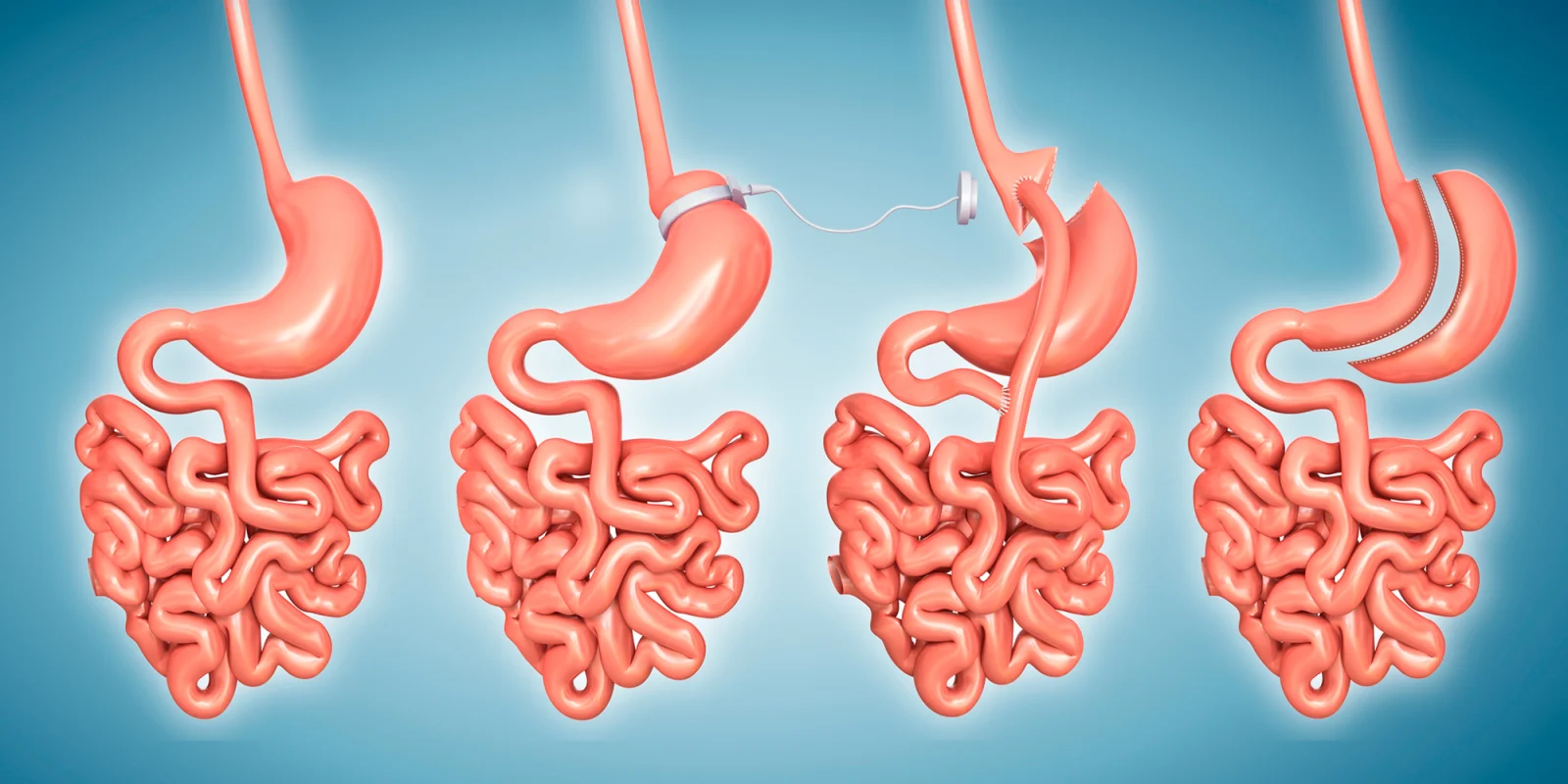
I was honored to moderate Dr. Jeff Mechanick’s meet the expert session on Postoperative Monitoring and Management of the Bariatric Surgery Patient at the AACE 2019 annual meeting. Dr. Mechanick started the session asking for a show of hands for anyone who had seen a bariatric surgery patient and virtually everyone in the room raised their hand. He explained that when he gave a similar presentation ten years ago less than half of the group raised their hand. The number of bariatric surgeries performed is increasing. In 2017 there were a total of 228,000 bariatric procedures performed. Approximately 53 percent were vertical sleeve gastrectomy and 18 percent were Roux-en-Y gastric bypass.
The Adiposity-Based Chronic Disease (ABCD) care model is a framework for obesity that emphasizes a complications-centric approach which determines therapeutic decisions and desired outcomes. ABCD is a new diagnostic term for obesity that identifies it as a chronic disease, identifies precise pathophysiologic mechanisms, and avoids the stigmata and confusion related to the differential use and multiple meanings of the term “obesity.” ABCD identifies a central role of lifestyle medicine but also recommends bariatric surgery based on the presence and severity of adiposity-based complications, as well as the degree of weight loss needed to ameliorate adiposity-based complications.
Dr. Mechanick discussed three core concepts for managing bariatric surgery patients. The first core concept is routine monitoring with aggressive case finding for nutritional and metabolic complications. The AACE Clinical Practice Guidelines for the Perioperative Nutritional, Metabolic, and Nonsurgical Support of the Bariatric Surgery Patient provide a comprehensive checklist for preoperative, early postoperative and late postoperative care of the patient having bariatric surgery.
Preoperative Checklist for Bariatric Surgery
- Complete H & P (obesity-related co-morbidities, causes of obesity, weight BMI, weight loss history, commitment, and exclusions related to surgical risk)
- Routine labs (including fasting blood glucose and lipid panel, kidney function, liver profile, lipid profile, urine analysis, prothrombin time/INR, blood type, CBC)
- Nutrient screening with iron studies, B12 and folic acid (RBC folate, homocysteine, methylmalonic acid optional), and 25-vitamin D (vitamins A and E optional); consider more extensive testing in patients undergoing malabsorptive procedures based on symptoms and risks
- Cardiopulmonary evaluation with sleep apnea screening (ECG, CXR, echocardiography if cardiac disease or pulmonary hypertension suspected; DVT evaluation if clinically indicated)
- GI evaluation (H pylori screening in high-prevalence areas; gallbladder evaluation and upper endoscopy if clinically indicated)
- Endocrine evaluation (A1c with suspected or diagnosed prediabetes or diabetes; TSH with symptoms or increased risk of thyroid disease; androgens with PCOS suspicion (total/bioavailable testosterone, DHEAS, D4-androstenedione); screening for Cushing’s syndrome if clinically suspected (1 mg overnight dexamethasone test, 24-hour urinary free cortisol, 11 pm salivary cortisol)
- Clinical nutrition evaluation by dietitian
- Psychosocial-behavioral evaluation
- Document medical necessity for bariatric surgery
- Informed consent
- Provide relevant financial information
- Continue efforts for preoperative weight loss
- Optimize glycemic control
- Pregnancy counseling
- Smoking cessation counseling
- Verify cancer screening by primary care physician
Early Postoperative Care
- Monitored telemetry at least 24 hours if high risk for myocardial infarction
- Protocol-derived staged meal progression supervised by dietitian
- Healthy eating education by dietitian
- Multivitamin plus minerals
- Calcium citrate, 1200-1500 mg/d
- Vitamin D, at least 3000 units/d, titrate to >30 ng/mL
- Vitamin B12 as needed for normal range levels
- Maintain adequate hydration (usually >1.5 liters/day)
- Monitor blood glucose with diabetes or hypoglycemic symptoms
- Pulmonary toilet, spirometry, DVT prophylaxis
- If unstable, consider pulmonary embolus, intestinal leak
- If rhabdomyolysis suspected, check CPK
Follow-Up Postoperative Care
- Visits: initial, interval until stable, once stable every 3-12 months
- Monitor progress with weight loss and evidence of complications each visit
- SMA-21, CBC with each visit (and iron at baseline and after as needed)
- Avoid nonsteroidal anti-inflammatory drugs
- Adjust postoperative medications
- Consider gout and gallstone prophylaxis in appropriate patients
- Need for antihypertensive therapy with each visit
- Lipid evaluation every 6-12 months based on risk and therapy
- Monitor adherence with physical activity recommendations
- Evaluate need for support groups
- Bone density at 2 years
- 24-hour urinary calcium excretion at 6 months and then annually
- B12 (annually; then every 3-6 months if supplemented)
- Folic acid (RBC folic acid optional), iron studies, 25-vitamin D, PTH
- Vitamin A (initially and every 6-12 months thereafter)
- Copper, zinc, and selenium evaluation with specific findings
- Thiamine evaluation with specific findings
- Consider eventual body contouring surgery
The second core concept Dr. Mechanick discussed was cardio-metabolic risk mitigation. This requires an acceptable pace of weight loss with long term weight maintenance. Target metrics include the BMI, A1c, LDL, CRP and blood pressure. The third core concept is lifestyle medicine for chronic disease prevention includes healthy eating, physical activity, tobacco cessation, alcohol moderation and sleep hygiene.
Dr. Mechanick presented three cases from his practice to highlight nuances in the postoperative management of the bariatric surgery patient. There were several teaching points found in each case. The first case identified the impact of severe nutritional risk in the bariatric surgery patient. Patients are at continual risk for vitamin and mineral deficiencies. Routine monitoring with additional evaluation for case-specific findings in necessary to identify nutritional deficiencies and to prevent their occurrence.
The second case discussed beta-cell defects and risk for LADA in bariatric surgery patients. Unresolved hyperglycemia after metabolic surgery should raise suspicion for LADA. There is an emerging role for GLP-1 agonists after bariatric surgery in those with problematic adiposity and/or with dysglycemia-based chronic disease.
The third case presented management strategies for patients who need bariatric surgery and also have thyroid cancer. Some patients may require staged bariatric surgery and/or staged thyroid surgery to minimize risk.
There is sufficient evidence to guide clinical decision making for preoperative, early postoperative, and late postoperative care of the patient having bariatric procedures. Endocrinologists should be aware of routine management protocols, efforts to mitigate cardiac risk, and durable lifestyle medicine approaches to manage chronic disease in patients who have had bariatric procedures.
The author (left) with Dr. Mechanick
References:
1. Mechanick, JM, et al. ADIPOSITY-BASED CHRONIC DISEASE AS A NEW DIAGNOSTIC TERM: THE AMERICAN ASSOCIATION OF CLINICAL ENDOCRINOLOGISTS AND AMERICAN COLLEGE OF ENDOCRINOLOGY POSITION STATEMENT. Endocrine Practice: March 2017.
2. Mechanick, JM, et al. Clinical Practice Guidelines for the Perioperative Nutritional, Metabolic, and Nonsurgical Support of the Bariatric Surgery Patient—2013 Update. Endocrine Practice: March 2013.