This is part of the Medical Humanities series on Op-Med, which showcases creative work by Doximity members. Do you have a creative work related to your medical practice that you’d like to share? Send it to us here.
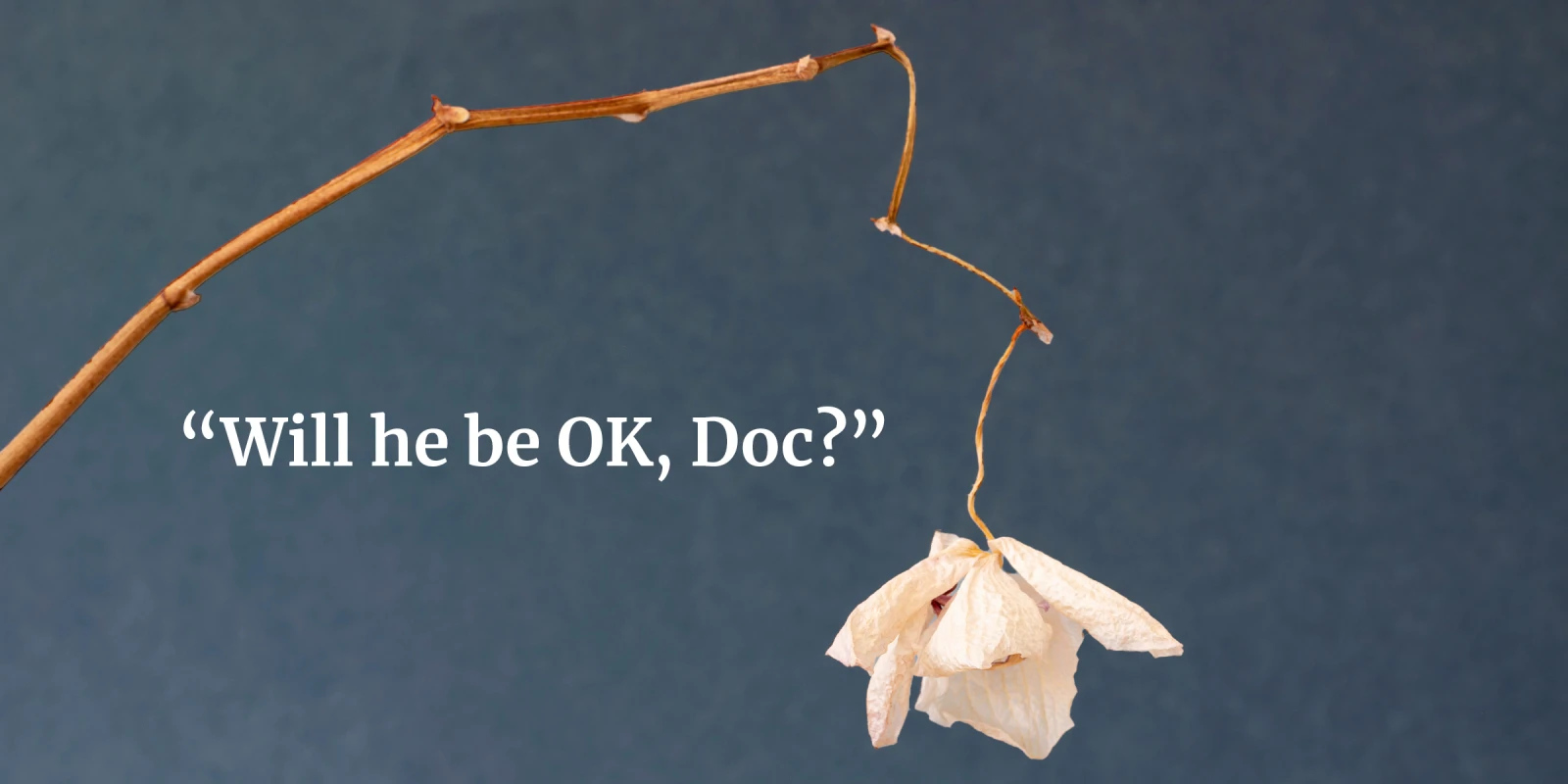
As I am leaving my office this evening, I see the last petal of the orchid struggling to hold on. The white petal with its withered brown edges looks like dirty old crumpled paper. The greyish crimson veins on it are faded. Even the evening sunlight streaming through the window pane is not enough to brighten it. I kneel on the ground to tenderly touch and feel the traces of its softness.
The touch transported me to the moment I first met Shirley, who gave me the white orchid. The visage of her in blue jeans and a white T-shirt, holding her 14-year-old daughter Katie’s hand, and leaning over the stretcher to kiss her husband Mike on his forehead as I wheeled him into the catheterization lab, came back to me as if it had happened yesterday. They did not know that 10 minutes later, Mike’s heart would be fibrillating like a fish out of water, wanting to stop altogether due to lack of blood supply.
“Will he be OK, Doc?” Shirley asked innocently.
“Mike is very sick. He is having a massive heart attack. I will do my best,” I promised her. I prayed silently, “Please God. Let it not be their last kiss.”
Mike looked sick with beads of sweat all over his temples and forehead. He was a handsome man with an angled jaw and greyish green eyes. Did I see fear or courage in those eyes? His heart was racing at 120 bpm. His blood pressure was dangerously low. His ECG showed tombstone ST elevations in all precordial leads. He was in cardiogenic shock. His otherwise sturdy body was in its most vulnerable state. He was only 40.
Becky, the tall, dark-haired scrub technician greeted us as we entered the cath lab. In a sweet, caring voice, she told Mike that we would take care of him. We were a team of four. Drew, the nurse, and Jack, the fluoroscopy technician, joined us, a highly competent team. Could we take care of him? Could the whitewashed walls and bright white lights of the cath lab keep Hades, the dark God of death, away?
As we transferred Mike onto the cath table and covered him in a blue sterile sheet, he started retching. Greenish, bilious vomit mixed with partially digested food particles covered the blue sheet. As Drew started cleaning up the vomit and re-draping Mike, I heard Mike’s soft, fading voice, “I am so sorry for vomiting. I am so sorry.” Who was this man so kind to be so apologetic when having a heart attack?
Mike’s fading voice coincided with the loss of organized regular green spikes representing the heartbeat on the monitor. His heart was in a quivering chaotic mess: ventricular fibrillation, a fatal rhythm. In a firm, loud, authoritative voice, I announced, “Call code blue!” Becky started chest compressions, pounding on his chest, trying to resuscitate his heart. Jack was immediately at the side of the defibrillator, ready to shock Mike. Becky stopped the chest compressions briefly and took a step back. “Everyone clear! Go ahead, shock!” I said, clearly.
Shock 1: Mike’s body jolted. No restoration of normal rhythm.
“Becky, continue chest compressions. Drew, give 1 mg of epinephrine and 300 mg of amiodarone,” I ordered in a loud but even tone. Adrenaline rushed into my veins, and my own heart raced, only much slower than Mike’s. I felt like a swan, looking calm on the outside but paddling furiously underneath the rough waters.
By this time, at least 10 people, all in blue, swarmed into the room in response to the overhead call. The room was dissolving into a chaotic mess matching the chaos of Mike’s heart rhythm.
Shock 2. Still no restoration of normal rhythm. Becky continued chest compressions.
Raising my voice a notch higher, over and above buzzing sounds of the alarms and multiple voices trying to talk at the same time, I announced, “This is Dr. Mallidi. I am in charge of running this code. Please report to me clearly after your task is completed.” Looking directly at the person to whom I would be designating the task, I said, “Dr. Brady, go ahead and intubate the patient. Becky, continue chest compressions. Drew, go ahead and give another 1 mg of epinephrine.”
Shock 3. Did not work.
The bounding of Mike’s pulse against my fingers was in rhythm with the timing of Becky’s chest compressions. No chest compressions, no pulse. Dr. Brady stood at the head of the cath table, trying to intubate Mike. As the camera of the fluoroscopic machine hovered over Mike’s chest, I only saw Dr. Brady’s balding head, and not his face. I heard his exasperated, raspy voice, “I can’t see anything; oropharynx is covered with vomit. Get me a glide scope, please!”
Shock 4. Mike’s heart was in unrelenting ventricular fibrillation.
With Becky still pounding vigorously on Mike’s chest, his whole body jerked with each thrust of compressions. I punctured his femoral artery and advanced a large sheath into it so I could have access to his heart vessels. Becky continued chest compressions while I tried to visualize Mike’s heart arteries on the fluoroscopic camera. Two of the three arteries were completely blocked.
Shock 5. More epinephrine, more amiodarone, and now, bicarbonate. Still in ventricular fibrillation. Dr. Brandy was struggling to intubate.
“We are going to insert the Impella,” I said. Impella is an external percutaneous pump that goes into the heart, and supports it while we work on restoring the blood flow in the two arteries.
Mike’s heart would stop any second now. The visage of Shirley and Katie holding hands and kissing him came back to me at that moment. What would I tell them? That beautiful young girl would be without a father — like me.
I felt Hades hover in the cath lab. A split second of prayer to God. A split second when I looked upwards at the bright light at the center of the cath lab in a gesture of prayer to my dad, and asked for help.
Dr. Brady announced, “Endotracheal tube is in.” I took a deep breath, and said, “Jack, shock again.”
Shock 6. This time I saw the disorganized squiggly rhythm convert into organized regular spikes — sinus rhythm.
There was a palpable sigh of relief from everyone in the room. Becky finally stepped back from Mike’s chest after close to 15 minutes of doing vigorous chest compressions.
Over the next two hours, we inserted the Impella into Mike’s heart for support and opened his blocked arteries with stents. He was transferred to the ICU in stable condition. Shirley and Katie were waiting to hear from me. I removed my heavy lead gown and headed first to the restroom before meeting them. The face in the mirror that stared at me was covered in circular, large red welts. I splashed cold water on my face and took a deep breath. I closed my eyes and saw my dad’s smiling face.
What was your inspiration for this piece?
This is the story of a young gentleman on the brink of death. His wife later presented to me a white orchid as a gift. As physicians, we often get bogged down by science, technique, and knowledge. However, medicine is an art. The white orchid, for me, symbolized purity and the power of love, prayer, and gratitude. This was my inspiration to tell this story and bring out the powerful emotions related to the art of medicine.
How long have you been writing? What got you started? How do you relate it to your medical practice?
I have been writing for more than five years now. I usually write opinion pieces using patient vignettes to bring out broader issues or problems in medicine. I write regularly for Medscape as a columnist and have also taken writing courses at Stanford in creative nonfiction.
All names and identifying information have been modified to protect patient and provider privacy.
Jaya Mallidi, MD, is an interventional cardiologist working in Santa Rosa, California. Her opinion writing can be found on Medscape.