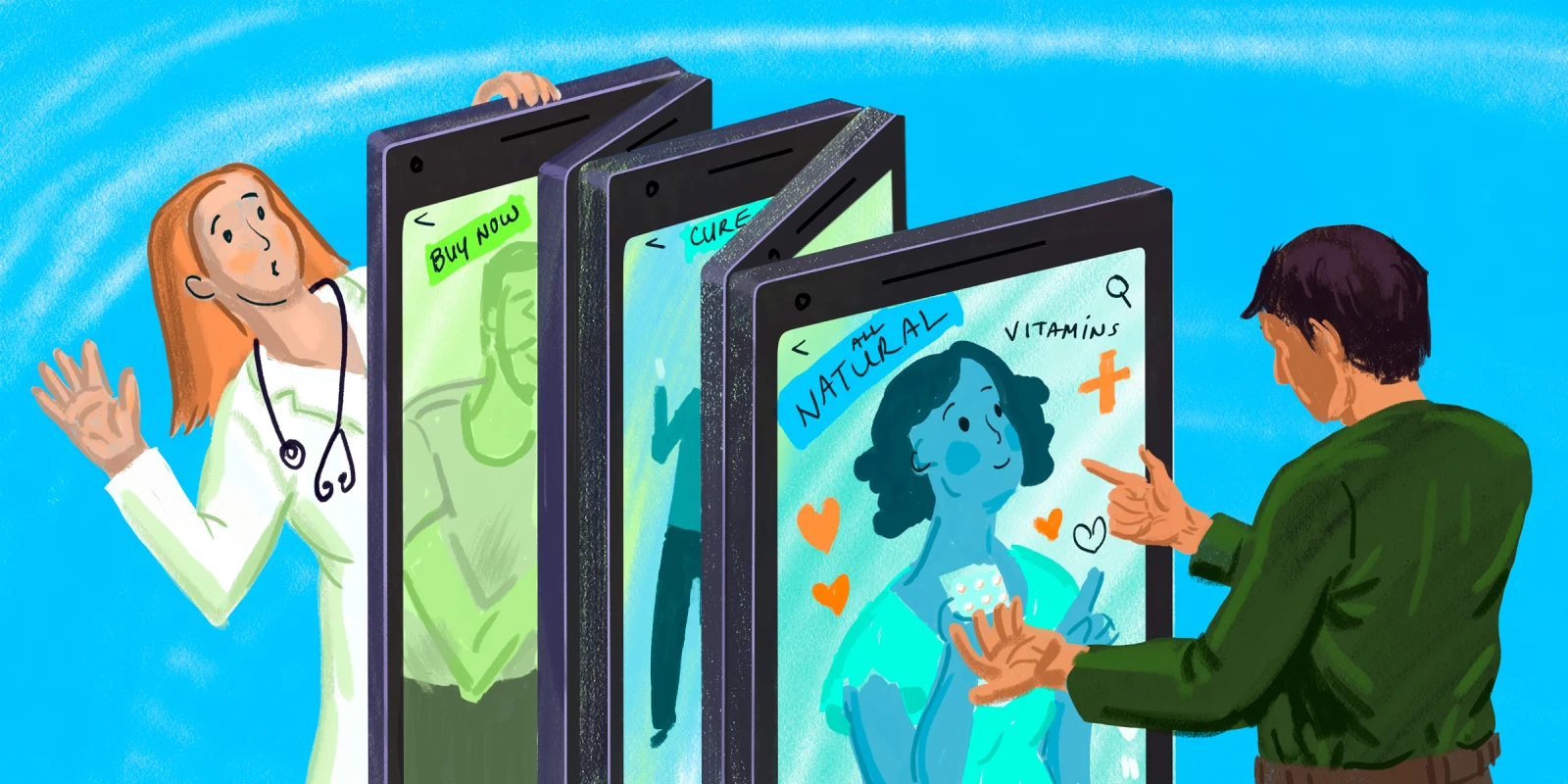
In this internet age, we APPs find ourselves confronting an unpleasant new problem: the rise of online “medical experts” with no actual training. Coupled with this trend is the fact that as APPs, our time slots with patients seem to get smaller by the day. This begs the question: What are we to do when a patient comes in with a binder of “evidence” from internet research into a rare condition they likely don’t have? How do we handle the request for expensive testing that we know won’t yield answers until more common tests are done to rule in a condition? How can we get through to patients who are inundated with messaging from TikTok influencers who imply that clinicians are withholding the magic pill that will make patients’ problems go away, or worse yet, are willfully ignorant? Below, I tease out the problem and offer solutions to rebuilding trust with patients in the limited time we have with them.
Loud Voices Promising Quick Fixes
Non-clinicians hawking products and cures is a tale as old as time, but the grip these self-proclaimed “experts” have on patients is stronger than ever before thanks to social media. In my GI clinic, I often have patients repeat things they’ve heard from influencers, particularly, “I am not interested in the medication that treats my condition, I only want natural cures.” Now, I am not anti-natural remedy or alternative treatments, but I am pro-evidence-based medicine. There are some great remedies that occur in nature (like peppermint for IBS pain) and may have become pharmaceuticals to treat disease (like IBgard). But when people with no training in a medical field are seen as more trustworthy and knowledgeable than patients’ own clinicians, it’s clear that something has gone awry.
To be clear, it’s not exactly patients’ fault that they are susceptible to this misinformation. It makes a degree of sense why patients desire to do their own research and seek out alternative voices. Medicine is short on time, doctors, and APPs; corporate medicine has relegated each appointment to one complaint only. People who are already paying high copays and taking time off work to discuss distressing symptoms are not keen to make six appointments to air out all their concerns. For all these reasons and more, patients may turn to the internet. Unfortunately, those online voices often tell patients exactly what they want to hear, with little regard for their actual complaints or for any contraindications. This means that patients can end up pursuing health paths that are not only ineffective, but dangerous.
I’ll give an example from my own practice. My patients with functional gastrointestinal issues will listen to recommendations from influencers that include enemas for constipation, adding over-the-counter digestive enzymes to their diet to improve leaky gut, drinking apple cider vinegar for their reflux, and fasting to help their belly woes. None of these are scientifically based and some of these can actually worsen the problem.
Of course, there are ways for patients to relieve symptoms and feel better. Working with a registered dietitian has been shown to be beneficial for patients with forms of IBS and chronic constipation. Pelvic floor physical therapists are amazing resources and can be very effective with patients who have pelvic floor dysfunction and concomitant constipation or fecal incontinence. There are medications for severe symptoms (e.g., linaclotide for constipation, eluxadoline for diarrhea) and plenty of lifestyle interventions that can really make a difference, such as adding in more fibrous foods, walking, and proper hydration. That said, it can be a lot of trial and error to find what works for the patient. And it takes months to really fully address the myriad of symptoms that will recur and remit.
Unfortunately, nuance doesn’t do well on the internet. And so influencers promise easy fixes, or blame one particular food for all GI woes, be it gluten, nightshades, dairy, or all vegetables and fruits.
Lack of Knowledge About How Diseases Work
In addition, influencers tend to promote two unhelpful ideas: a) that illnesses have a “root cause,” and b) that a diagnosis is knowable and lifechanging. Sometimes in medicine, we may not know the root cause, but we do know what will alleviate the symptoms. Sometimes the root cause of a disease state is very clear to us, as in ulcerative colitis. Sometimes you just need to avoid garlic because it makes you gassy and your distention is gone. And receiving a formal diagnosis of IBS doesn’t change that recommendation.
However, for some patients, a lack of a formal diagnosis can feel like a sign that their clinician isn’t capable. These patients worry that if an APP can’t give them a diagnosis within two visits, then that APP is part of the ‘establishment’ and doesn’t care about them. Sadly, there are plenty of unvetted “experts” who will feed on these patients’ anxieties and fears. I have encountered numerous videos of non-clinicians accusing the medical establishment of bowing to big pharma and hiding the “true cure,” which generate comments involving negative impressions of all clinicians and accusing all clinicians of not listening and of not knowing the symptoms of chronic disease. While I sympathize with patients who are struggling with their symptoms and seeking out support, I worry about what it means for their health in general if they begin to adopt an anti-clinician attitude. Though venting can be beneficial, what happens when any decision a clinician makes, no matter how legitimate, is deemed suspect? Will a patient stop going to treatment?
As an APP working in a field where “cures” are hard to find, I am frustrated for my patients as much as they are frustrated. I too want to know what’s going on with them — but it can be hard when the trust isn’t mutual. Add the health anxiety generated by “experts” with no clinical training and we clinicians are doing lots of reassuring and over-explaining, which though important can take time away from working up symptoms.
Over-emphasis on Zebras
Another common theme in online “expert” videos is people discussing their very rare conditions (and hawking pseudoscience fixes). Patients see these videos, hear the list of symptoms, and think they have them too — even when it’s extremely unlikely. Now, are there patients who show up with vague symptoms that turn out to be an odd presentation of an uncommon illness? Sure! I don’t mean to imply otherwise, but as the adage goes, “When you hear hooves, think horses, not zebras.” Patients aren’t necessarily trained to think this way, however. They believe they have a zebra, and may not trust you if you tell them otherwise. This is partly because of the general lack of shared baseline knowledge among clinicians and patients. For example, I know that if as a primary care APP, I order a thyroid test and the TSH is normal, the patient likely doesn’t have thyroid disease. But a patient may listen to an internet “expert” who says that I should have ordered a full panel, autoantibodies, and multiple other specialized tests that aren’t necessary with a normal TSH — and then feel dismissed, hurt, and confused when I don’t do that. As a result of all of these tensions, it’s a constant uphill battle to build a trusting relationship with a patient so that when you don’t do something they expect, like order an obscure test, they are confident that you are not going to abandon them.
How to Rebuild Trust with Patients
That said, there are ways to get patients to trust you again. My best advice for those encountering these issues with patients is the following:
1) Be transparent whenever possible. If someone asks you why you did or didn’t order a test, explain. You don’t need to take up the whole appointment with explanations but a little candor can go a long way.
2) Educate your triage schedulers to ask questions about the nature of the visit. Sometimes a patient will come in with something straightforward like heartburn; other times someone will come in who has high expectations and is seeking a different opinion on their symptoms than the ones they’ve already received from multiple other clinicians. With the latter patients, make sure to schedule enough time for the appointment to sort out if anything was actually missed or if their expectations are unreasonable. (And remember to keep an open mind.)
3) Be patient. It’s hard. It can be REALLY hard, but these patients are coming to you because others failed to take the time to hear them. Most people who like me as their APP will commonly remark to my colleagues that I listen. It’s been a lesson I learned the hard way. I didn’t always listen, I didn’t always check my bias. Use my experience for your gain.
4) Be open to checking out the information patients bring you and if it’s not scientifically sound, explain to them why in a way that doesn’t make them feel ashamed or dismissed, like they knocked over the wedding cake. Just the other day I had to explain why the food sensitivity testing isn’t a validated test in the medical community, but working with a dietician and keeping diaries are valuable and reliable ways to find trigger foods without resorting to throwing out your pantry.
5) Learn to say “I just don’t know,” because sometimes we don’t. It isn’t a failure in our efforts; some things aren’t solvable and some patients will move on until they find the one clinician that’s willing to do things their way. It’s OK. You’re still a good person and a good provider of care to people. It’s not personal.
6) Instead of telling patients they shouldn’t be listening to outside voices, meet them where they are. Lead patients toward credentialed professionals who make online content, and explain how they can identify them. I keep a list for my patients of GI experts, reference books, and sometimes even a podcast or two that I feel is good information to share.
Ultimately, it is our responsibility as clinicians to educate and sometimes even learn new things in an effort to fight the good fight. Will you and your patients both get frustrated at times? Probably, but at the end of the day the effort is worth knowing you helped someone alleviate their symptoms and feel even a little better and leave with more knowledge about their condition than what they came to you with.
How do you work to temper patients’ expectations around cures, zebras, and the like? Share in the comments.
Allison Falin is a nurse practitioner in Maryville, TN. She enjoys weightlifting, hiking in her nearby Smokies, and just being outside. She has practiced as a NP for 11 years and RN for a cumulative 27. She and her husband have three adult children and four dogs. She is on threads as @alliefnp. Allison is a 2024–2025 Doximity Op-Med Fellow.
Illustration by Jennifer Bogartz