
Dr. Webster Pilcher, M.D., Ph.D., is the Chairman of Neurosurgery at the University of Rochester Medical Center and the Clinical Director of the Program for Translational Brain Mapping.
As soon as he received the case, Dr. Webster Pilcher knew this could be the surgery of a lifetime. For patient Dan Fabbio, it was.
As a musician who was working towards his master’s degree, Fabbio couldn’t imagine a life without music. And, yet, the possibility was very real.

In the spring of 2015, after weeks of seizures and hallucinations, Fabbio was diagnosed with a brain tumor. Fortunately, it was benign. Unfortunately, it was located in the right side of the brain — potentially near the region specialized in music.
That’s where Pilcher and his team came in.
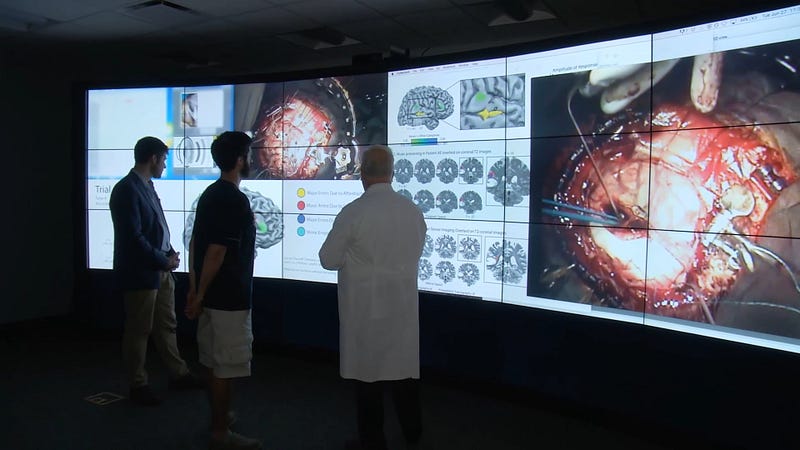
At the University of Rochester Medical Center, Pilcher and his colleague, Brad Mahon, Ph.D., co-lead the Program for Translational Brain Mapping. This program combines functional MRI (fMRI) scanning with live electrical stimulation to create patient-personalized brain maps. By having patients engage in activities, such as reading or singing, during these procedures, the team can precisely pinpoint the activated structures of the brain. Utilizing these maps as a guide for surgery, Pilcher hopes to preserve the critical functions most important to a patient, while simultaneously advancing scientific knowledge of the brain.
AS: What are your personal and professional intentions behind the brain mapping program?
WP: When I came here 20 years ago, I was very interested in mapping the brain using electrical stimulation. It’s a very effective technique, but it’s limited in so many ways. There’s only so much you can do in the short time that you’re in the operating room.
Then, I quickly realized that the cognitive sciences department across the street was using functional MRI scans to map the brain in a similar manner. So, I recruited Brad, a cognitive scientist from Harvard, and we tried to envision how we could bring this science into the operating room, not only to improve outcomes for patients, but also to help us advance the field.
On a more personal level, I’ve gotten to that point where you sit down with a patient, you learn their story, you meet their family, and you easily put yourself in that patient’s shoes. You really start to see the human dimension.
As an MD/PhD, your inclination is to leverage all of the scientific aptitude you can to create a better human outcome for the patient. The excitement and intellectual stimulation of working with a great scientist, like Dr. Mahon, the stimulation of being able to bring all of that science into the operating room, to be innovative in how we map the human brain, and to think that, as a surgeon, I can make a small contribution to the advancement of cognitive science — all of these things are, frankly, very enriching.
You get the benefit of a great human outcome, the benefit of being able to reassure patients and their families that they will be the same person after surgery, you get the opportunity to continually challenge yourself to advance the science of brain mapping in neurosurgery, and you get to work with intelligent, creative scientists. I can’t imagine a more gratifying experience for any professional.
While the team had experience in mapping language, speech, and mathematics, this was their first time mapping music in the brain. So, in preparation for Fabbio’s tumor removal, Pilcher and Mahon enlisted the expertise of music professor Betsy Marvin.
Together, Marvin and Fabbio composed simple musical melodies that Fabbio would then be instructed to repeat and interpret during his fMRI scans. In this way, Pilcher and Mahon created a three-dimensional diagram of his brain, highlighting the exact portions they would need to salvage.
AS: What did you find through the fMRI brain mapping?
WP: As Dan was humming back different phrases and melodies, […] we were able to map the area of the brain specialized for music. [We] found that, at the top edge of the tumor, there was a thin strip of brain cortex that was specialized in music. And, the tumor was pushing into it and beginning to displace it. It was obvious that the tumor was right in the area that was responsible for music.
So, we told Dan, ‘we would love to take the entire tumor out, and we think we can do it with you awake.’ This would be very different from most traditional surgeries. In this operation, we couldn’t completely map the brain without the patient’s complete engagement during surgery. The likelihood of Dan being able to be the same musician after surgery as he was before was very much dependent on that.
After six months of analysis and preparation, it was finally time to remove the tumor. Through “sophisticated computer technology” and “millimeter precision,” Pilcher was able to project the fMRI-enabled brain map onto the surface of Fabbio’s brain. To verify the accuracy of this map, he then stimulated segments of the brain, while Marvin constantly engaged Fabbio in musical tests. Just as the team suspected, Pilcher found that the tumor was directly adjacent to the region responsible for the interpretation of music.
Nevertheless, slowly but surely, the tumor was dislodged. To confirm the surgery’s success, however, Fabbio was tasked with one final feat — a saxophone performance, “the highest level of his personal music expression.” Marvin and Fabbio had previously worked to revamp a simple Korean folk song that he was to play at this moment. After placing the saxophone in his hands, brain still exposed, the entire OR held its breath.
Fabbio played the song flawlessly. And, at that point, the entire room burst into applause.
AS: What did it feel like after Dan performed that piece in the operating room?
WP: It was a little bit like hitting a homerun in a baseball game. We had thought about this operation for months; we had planned very carefully for it. For that brief moment when we were applauding him, it was very rewarding. There were probably 15 people in the OR, all of whom were engaged with the surgery. But, like any moment of triumph, it quickly turns back to reality. It takes an hour and a half to close the brain back up and get [a patient] out of the OR, so we had to get back to work. But that moment — hearing him play the instrument — is one i’ll never forget.
While it took a few weeks for Fabbio to fully recover, his surgery was a success. Afterward, he was able to return to his life in music.
This case was also a significant hallmark in Pilcher’s career, and he hopes to apply his findings to future patients.
AS: What were the key findings of this case, and how will these discoveries further subsequent operations?
WP: We confirmed, for the first time, that the fMRI mapping of music in the brain was accurate, as proven by the electrical stimulation experiments in the OR. With regard to musical organization of the brain, we learned that this area in the brain is very similar to an area that participates in aspects of language. The music area of the brain is organized in a similar way as the verbal language part of the brain, which, in a simple-minded way, makes sense, because music is an expression of human thought and language. We’re eager to put that knowledge to use, not only in our research, but also in future operations, as we have the opportunity to encounter patients with musical talent. I think this will be an incredible way for us to push the frontiers of brain mapping forward.
We also confirmed that, in an operating room setting, we can have a musician playing an instrument and humming phrases in a way that was practical. It was a demonstration that, by partnering with a musician, such as Betsy Marvin, and by amalgamating neuroscience, surgery, music, and other fields, we can perform operations that have never been done before.






