Home hospice is a subject that has been explored greatly. The focus on death and dying and inadequate funding often take a front seat in many of the conversations, rightfully so. And yet, hospice is also about celebration of life and connection. Below, I share lessons in the latter I learned from working with an interdisciplinary home hospice team as an inpatient and outpatient clinician.
1) Cultural Connection
I once had a hospice patient with pancreatic cancer. Care at this point was a balance between providing relief from the dyspnea and pain she was experiencing and also having a clinician embrace her own offerings. The concern that day was nausea. The ondansetron the patient received had provided some relief, she said. She then asked, Had I used smelling pods before? No, I said. The patient signaled to her dresser across the room for me to bring a container over. As I walked over she pointed out each and every picture of her children and how proud she was of her granddaughter who was now a physician abroad.
When I returned, the patient opened the box and held up a single pod to my nose. It felt like a lightning bolt shot through my senses — my reaction was so visceral. She laughed as she explained she much preferred these that she had used while growing up in Trinidad. I could understand why: it was one of the strongest smells I had ever experienced. She said she often used these to help with nausea. I had no doubt they worked as I felt as though my entire palate had been wiped out. My conventional alcohol swabs for nausea paled in comparison and I felt rather sheepish having offered such a paltry substitute.
My time with this patient felt like a game of show and tell. From our Eastern-centric “medicine box” I would offer relief for her ailments and in turn she would share her Trini alternatives. Ultimately, she embraced our conventional offerings, but it was important for her to share pieces of her culture. There was never an expectation of myself embracing or accepting the remedies she would present, but I knew she valued not being dismissed.
The ability to spend more time with a patient and to witness a demonstration of their own remedies feels unique to home hospice. I never had time for that in the clinic, but in home hospice, where the emphasis is on what brings the patient relief and joy, spending such time is crucial. Without sounding patronizing, while we focus on evidence-based medicine for guiding our decision-making, if smelling pods or floral drinks makes the patient happy, then letting them share that is our main objective. There is a vulnerability to a patient revealing a piece of their culture knowing full well that it could be shut down or dismissed by their clinician, and that is something I don’t take lightly.
2) Unvarnished Emotionality
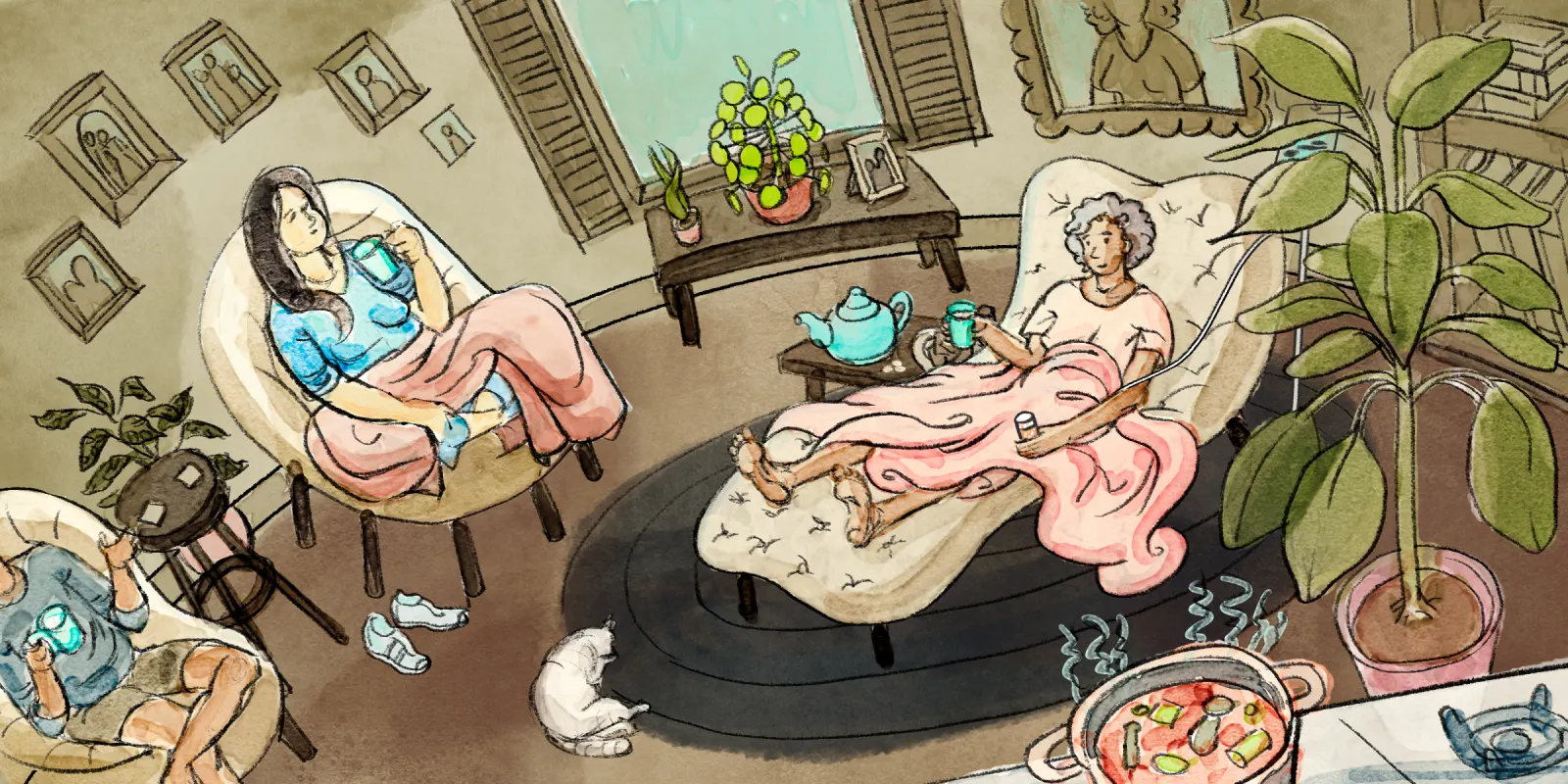
Despite the cushioned seating that furnishes waiting areas, even the coziest of medical offices have an air of sterility and coldness that carries forth to the interaction. There may even be an overall sense that the clinician is the head of house and a patient is invited into the space.
I have found the dynamic shifts during home hospice visits. The clinician becomes a visitor in a foreign territory. Small gestures such as taking off one’s shoes and hanging one’s coat in another’s space inherently make the encounter feel more intimate. The literal removal of the outer layer leaves a smaller distance between oneself and the patient.
During my time visiting patients in home hospice, I noticed that being in a familiar domain seemed to provide patients with not only a sense of physical comfort, but also one of psychological safety. For patients who have to endure an hour-long subway ride after a visit, the odds of breaking down emotionally are rare. But in the comfort of one’s own home, with one’s own blankets to absorb the fear, the tears and memories flow.
I was surprised to see the emphasis and overwhelming spirit is one of joy. While death and dying sits in the background like a proctor eyeing the exam room, it does not take precedence over the whole affair. The focus is on what matters most. A social worker I spoke to shared my observations, and noted that reframing to patients that it’s not about how much time we have left, but how we utilize the time we have left has helped them process their experiences.
Utilizing time can look like so many things. Hanging out with family. Mending relationships. I often reflect on my older patients and hospice care patients and how much I long to start a project to help carry out their desires. Whether it’s legacy work creating a printed memoir, or putting on a Carnival celebration, this is a goal I hope to accomplish for at least some of my patients in the coming year. After all, like I say to my patients, it’s never too late to do something great.
3) Family Appreciation
Sometimes, I’m not able to have uninterrupted time with my patients during a home hospice visit. Eligibility for home hospice often requires beyond the services provided that family or friends be available. They are often the narrators of the scene. I’ve learned many a chili recipe and watched much sancocho almost overflowing in the pot — perhaps an apt metaphor — as a caregiver shares how a patient is doing. During these interactions, the rigid type A adherence to the clock I feel in clinic settings becomes an impediment. Rather, slowing down and absorbing the stories is the key. After all is said and done, a family will remember the care and interactions you had with them — not how efficiently you managed to keep the visit going.
This is not to say that the norms of the clinic setting cease completely. Some of my fellow clinicians explained to me that working with these patients and their families felt like a constant cycle of death and reset, without any time to process. I asked them what could help, and they told me that having a dedicated debriefing time to talk about difficult or touching cases would go a long way. Reflecting on those who have died and leaving space to share any lingering thoughts is a helpful exercise in general, whether we are doing inpatient, clinic, or home visits. We need more of this in order to prevent clinicians from burning out and feeling mechanized in our actions.
Ultimately, home hospice care is not a uniform experience, and there are still many barriers to bringing care up to par for each and every patient. But it’s important to recognize the great work that these teams do. Home hospice is truly a glimpse into a patient’s soul. An invitation not taken lightly. An intimate experience that I otherwise as a clinician would not have experienced. The existential and spiritual conversations I joined in that were intended to feel cathartic to patients, were, to my surprise, also refreshing for myself. It is in these moments centered around the role of death in life that we pause: we get to know ourselves, and in so doing we see the patient not as a patient, but as a fellow person.
What have been your most memorable lessons from caring for hospice patients? Share in the comments.
Dr. Helen Chen is an integrated Geriatrics and Hospice and Palliative Care Fellow in New York City. She is a food lover and is always on the look out for the best bahn mi, falafel, and tacos (although is allergic to red onion and avocado!). Her instagram is @gouda_vs_evoo. Dr. Chen is a 2023–2024 Doximity Op-Med Fellow.
Illustration by Jennifer Bogartz