This is part of the Medical Humanities series on Op-Med, which showcases creative work by Doximity members. Do you have a creative work related to your medical practice that you’d like to share? Send it to us here.
The situation of people experiencing homelessness in Seattle has become the first thing that my visitors from around the U.S. or abroad notice. I have no novel solutions to this crisis, but I know that each person is an individual and not just a statistic. Some are mentally ill, others are addicted to drugs or alcohol, some just had a run of bad luck, and many prefer the homeless lifestyle to a more settled one. I came to know one such person, “Robert,” well, and his story makes me more sympathetic to the homeless population and more skeptical of many policy proposals.
I came to know Robert as a unique person. I knew little of his history when we first met on a referral from a social worker friend who knew I did pro bono operations. Robert had congenital facial deformities. His initial appearance was unusual — a short, Native American with a hunchback, wearing a trucker’s cap embroidered with the Confederate flag. He appeared to have a variation of hemifacial microsomia with microgenia, malar hypoplasia, and an extremely deviated nose. As well, he suffered from a cervical spine deformity. He was said to have borderline mental abilities, but he was able to read a little. His personality was attractive in a disarming way. Robert was charismatic in a way that had to be experienced. He was medically indigent at the time, but thanks to the generosity of our hospital, I was able to perform procedures to reconstruct the nose, chin, and malar complex.
He was discharged in good condition for routine follow-up. Two days later, I received a call from the county jail that he had been arrested and was in custody there. He had walked out of a store in downtown Seattle with a small television set, and the owners called the police when he refused to stop. I spoke to the nurse at the jail, where he subsequently received excellent postoperative care and was then released. The police assumed he was mentally deficient and not responsible – perhaps, but he did manage to get himself admitted to a comfortable infirmary with good nursing care for his recuperation.
I saw him several times in the postoperative period. He always opened our conversations with “Hi Doc,” a touch on my shoulder, and a wink. He healed well and had a good result. His social worker at the public health clinic traced his history back to a Blackfoot tribe in Canada. Both parents were alcoholics and died when he was young. He moved from orphanage to orphanage and school to school. He had periods of sobriety followed by alcohol and other drug abuse.
I met him one last time several years after his surgery. I was walking along the waterfront when he appeared in front of me. He recognized me, thanked me, and then asked if I had any change. I gave him some, and he walked away with his curious smile.
The clinic called me a few months later to tell me Robert died from a heroin overdose. We helped Robert with his facial deformities but failed him in a larger sense. The social workers had done their best, but he wasn’t willing to undergo drug or alcohol treatment — nor did he want to be in a shelter. He seemed comfortable with his life on the street, as difficult as it seemed. We, as physicians, prefer to categorize and diagnose people and then triage them to the best treatment centers. It is probably a good model overall for our homeless population, but some don’t want to follow our guidance. Patients, like Robert, can be stubborn and difficult, even frustrating, but they nevertheless insist on following their own path. Even though we ultimately failed Robert, I will never forget him.
What was your inspiration? Did other creative works, if any, influence your creation of this piece?
I have always enjoyed William Carlos Williams and his doctor stories.
How long have you been doing this activity? What got you started?
I was writing before I became a surgeon. Writing is a way to communicate with others as well as explore my own life. I have been interested creative writing since high school — I mainly compose poetry, but I also write some prose.
Is there anything else you'd like to tell us about your involvement in or views on arts in medicine?
I believe the art of medicine is often lost in the business of medicine. My main surgical book is the "Art and Craft of Facial Rejuvenation." Although medicine is and should be science-based, a good aesthetic sense and good craft are also crucial for excellent outcomes in facial plastic surgery
Why did you choose this medium? What interests you about it?
I love photography and poetry, but short prose is the best way to tell a story. I have always composed creative writing, both prose and poetry.
How does this submission relate to your medical practice?
Robert was a patient of mine. He was a unique patient that I treated pro bono.
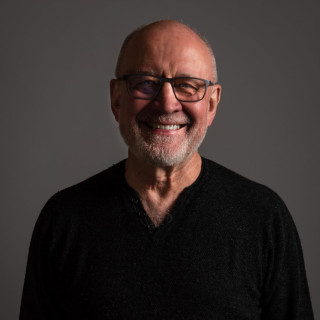
Wayne Larrabee is a facial plastic surgeon in Seattle. He has published poetry and photography as well as over 250 medical articles and three major medical texts. He has been president of the major medical boards and societies in facial plastic surgery, including the AAFPRS, ABFPRS, ABOto, and IFFPSS. He is the director of Global Surgical Outreach, which provides reconstructive surgery to children in less-developed countries.
All names and identifying information have been modified to protect patient privacy.