I arrived at work after a restful weekend to find an unexpected lab result in my desktop on Monday morning. The looming lab was an elevated platelet count of 600. The result belonged to my young newly abstaining alcoholic patient. The lab was drawn in the second week of the patient’s alcohol withdrawal and revealed a concern for a clot risk.
I arrived at work after a restful weekend to find an unexpected lab result in my desktop on Monday morning. The looming lab was an elevated platelet count of 600. The result belonged to my young newly abstaining alcoholic patient. The lab was drawn in the second week of the patient’s alcohol withdrawal and revealed a concern for a clot risk.
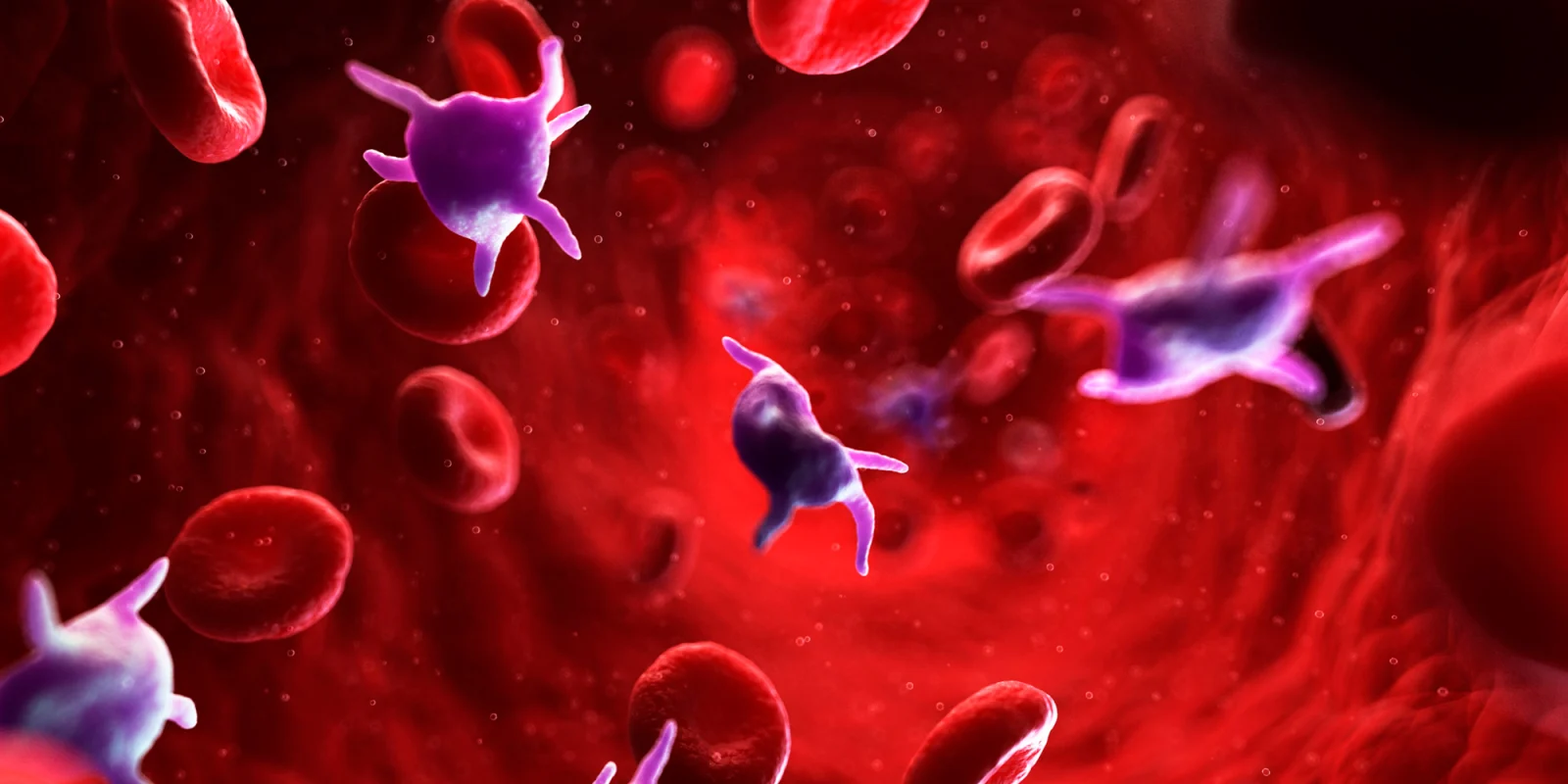
Usually, in my practice, I have a trend to observe low platelet counts in my alcoholic patients due to the fact they seek medical care late in the disease progression and many have early or later stages of cirrhosis and liver fibrosis due to splenic sequestration of platelets. Often, I see platelet counts of 30–40. This thrombosis of 600 was marked and was the only abnormal lab of the work-up in my young patient. What was going on?
Evidence points to a pathophysiology of a high platelet count approximately 2–4 weeks after the last drop of alcohol. The risks with the thrombosis is thicker blood and higher clot risk. Pulmonary embolism and DVT are common in hospitalized alcoholics undergoing withdrawal but has mostly been contributed to the comorbidity of cardiomyopathy as well. Thankfully my patient was not on oral birth control or hormonal therapy but her condition warranted a prescription for baby aspirin and information on staying hydrated and monitoring for blood clots.
In general, increased alcohol intake is associated with thromboembolic disease and cerebrovascular insults. Both hypertension with elevated platelets occurs during alcohol withdrawal. In contrast, during chronic alcohol intake thrombocytopenia is prevalent. The pathophysiology of the platelet aggregability is due to an increase in ADP and adrenaline as agonists and changes in collagen and ristocetin. The triggering factors are DNA damage and mitochondrial poisoning which leads into the above mentioned cascade.
In a landmark study by Fink et al. in 1983, the hyper-aggregable state of the platelets was accomplished in 7–10 days after the last alcoholic drink. However, after 14 days of alcohol abstinence the platelets declined by 15%. Cerebral blood flow was noted to decrease by 30% during withdrawal. Even non-alcoholics recovering from a binge drinking experience had rebound thrombosis. The platelet aggregability is influenced by the influx into the circulation of newly formed thrombocytes and the resulting increased platelet size. In contrast, the PGE1, the aggregation inhibitor, surprisingly falls.
Clinically, my patient was aware of her risk factors but was also reassured that this risk will decrease and will improve shortly. Sure enough, the platelets on recheck returned to normal range at one month.
I believe with an increasing prevalence of alcoholism and an aging population with comorbid factors that in the next decade clinicians will need to pay attention to monitoring platelet levels in alcoholism and consider individual risk factors for increased clotting risk. In a nutshell, this was a helpful review of the pathophysiology of thrombocytes in alcoholism.
Connie Lapadat, NP, is a family nurse practitioner in El Cajon, CA. She is a 2018–19 Doximity Author.
Image by Science Photo Library - SCIEPRO / gettyimages