
At this year’s American Society of Plastic Surgeon’s meeting I had the honor of presenting on the World’s first panel on shared decision-making in breast reconstruction. It was a unique panel at the ASPS, the only one composed of plastic surgeons and patient advocates.
Shared decision-making occurs when the health care provider and patient work together to make a health care decision that is best for the patient. The optimal decision takes into account evidence-based information about the available treatment options, the provider’s knowledge and experience, and patient factors including their values and preferences.
The “information exchange” that occurs between the patient and physician is completely different to the paternalistic approach many of us witnessed during our training, ie “this type of breast reconstruction is the best. That’s what we’re going to do for you”.
The “Informative” approach to decision-making provides the patient comprehensive information, but unlike shared decision-making, does not consider the patient’s values or preferences. Shared decision-making also incorporates the biological, sociological and psychological factors the patient brings to the table.
A recent study showed less than half of patients undergoing mastectomy made a high-quality breast reconstruction decision based on their self-reported desires. ‘High quality’ was defined as ‘having knowledge of at least 50% of the important facts and undergoing treatment concordant with one’s personal preferences’. In my opinion, shared decision-making can help us do significantly better than this.
Access to health information on the internet and via social media is changing the patient’s role in healthcare. People are advocating for themselves more and becoming more involved in their health care decisions than ever before.
Multiple studies across several medical and surgical specialties show shared decision-making offers many benefits to both the patient and physician:
· Improves patient education
· Decreases patient anxiety
· Decreases decisional conflict
· Helps set appropriate patient expectations
· Improves patient satisfaction
· Improves patient outcomes
Decreasing decisional conflict means the patient is less likely to seek a second opinion because of insecurity, and it also decreases medical malpractice risk.
Improving patient outcomes and satisfaction can also create extremely positive secondary effects on the surgeon’s practice from a marketing perspective. Happy patients can be very effective advocates for a specific procedure or the entire practice.
Shared decision-making is also intrinsically quite rewarding. In addition to being effective and ethical, it enables the delivery of high quality, patient-centered care.
The SHARE approach breaks down shared decision-making into the following simple 5 step process:
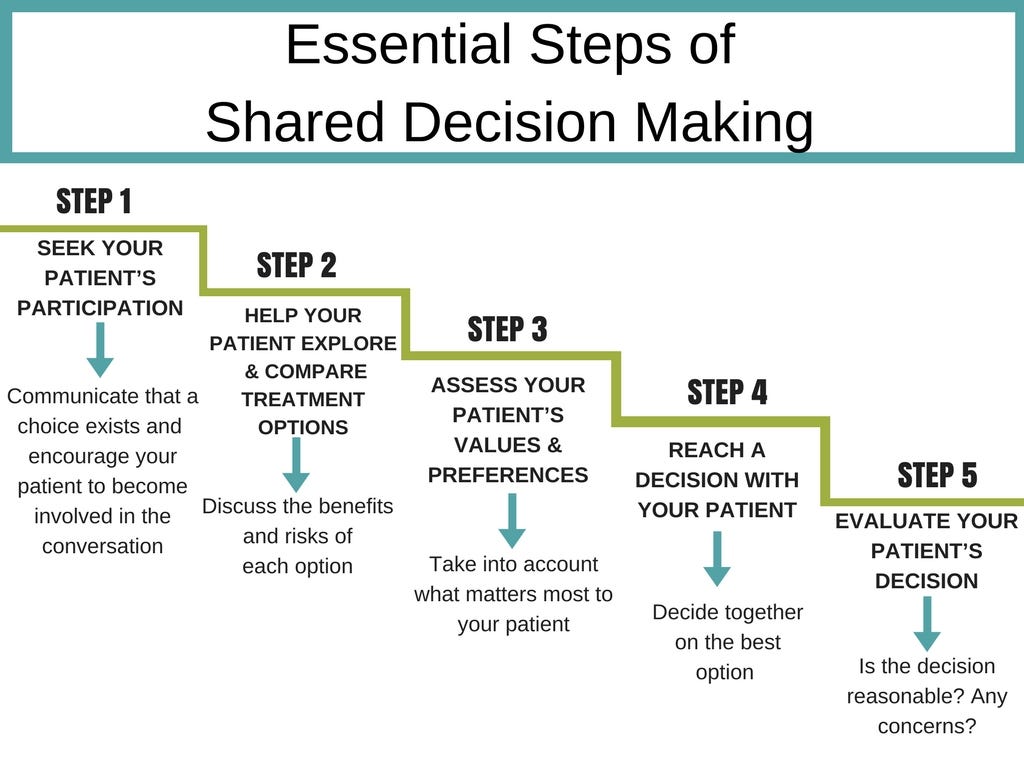
Step 1 encourages patient involvement and autonomy. However, it is important to acknowledge that breast cancer can make people vulnerable and insecure. Assuming — or even imposing — patient autonomy can lead to an underestimation of the patient’s vulnerability and an overestimation of their ability to make good decisions. In some cases, an appeal on autonomy can therefore be a burden. The main goal of shared decision-making is not to always have patients make autonomous choices, but to provide high quality patient-centered care based on the level of involvement the patient is seeking.
The various breast reconstruction options and associated risks are reviewed during step 2.
Step 3 defines the patient’s priorities by listening to what’s important to them. What do they need to make the reconstruction process worthwhile for them? For example, are they merely seeking to be able to wear a bra, or do they expect to look better than before in a bikini? How do they feel about implants? How do they feel about potential donor site scars? How important is sparing the nipple-areola? Do they know the mastectomy will likely rob them of most, if not all, of their breast sensation? How important is sensation to them?
Step 4 involves discussing how their preferences favor certain options while taking the overall clinical picture into account. Patients may hold a view that one reconstructive option fits their lifestyle and values better than another. This view may be different from the surgeon’s. Shared decision-making recognizes the patient’s right to make these decisions, ensuring they are fully informed about the options they face, and the likely consequences both short- and long-term.
Step 5 is assessment of the treatment plan. Is the plan medically appropriate and reasonable? Is it compatible with other anticipated breast cancer treatment?
While shared decision-making has many benefits, it has not been widely adopted by the medical community. Cited reasons include increased workload and the fee-for-service model. There is no-doubt that this approach can increase emotional effort and at least initially, may prolong the length of consultations. However, as with a new surgical technique, familiarity improves comfort level and efficiency. Regardless of reimbursement model, improved patient outcomes and satisfaction can only help your practice.
While the case can certainly be made that some procedures have proven advantages in certain clinical situations, there is no global “right” choice for breast reconstruction and we must acknowledge that every patient’s needs are different. Surgeons and patients must discuss patient values and preferences while also assessing what is medically appropriate and reasonable. Shared decision-making not only improves patient satisfaction and outcomes, but is also a very effective and ethical approach in ensuring our patient’s preferences and values are considered when planning breast reconstruction.
Author Bio:
Dr. Minas Chrysopoulo is a board certified plastic surgeon, breast reconstruction surgeon and microsurgeon at PRMA Plastic Surgery | Center for Advanced Breast Reconstruction, and also the creator of the Breast Advocate App, a shared decision-making app for breast cancer surgery and breast reconstruction. He has dedicated his professional life to advocating for breast cancer patients and believes shared decision-making between the surgeon and patient is crucial in achieving the best breast reconstruction outcomes.







