Dr. Lisa Friedman is a 2020–2021 Doximity Research Review Fellow. Nothing in this article is intended nor implied to constitute professional medical advice or endorsement. The views expressed in this article are those of the author and do not necessarily reflect the views/position of Doximity.
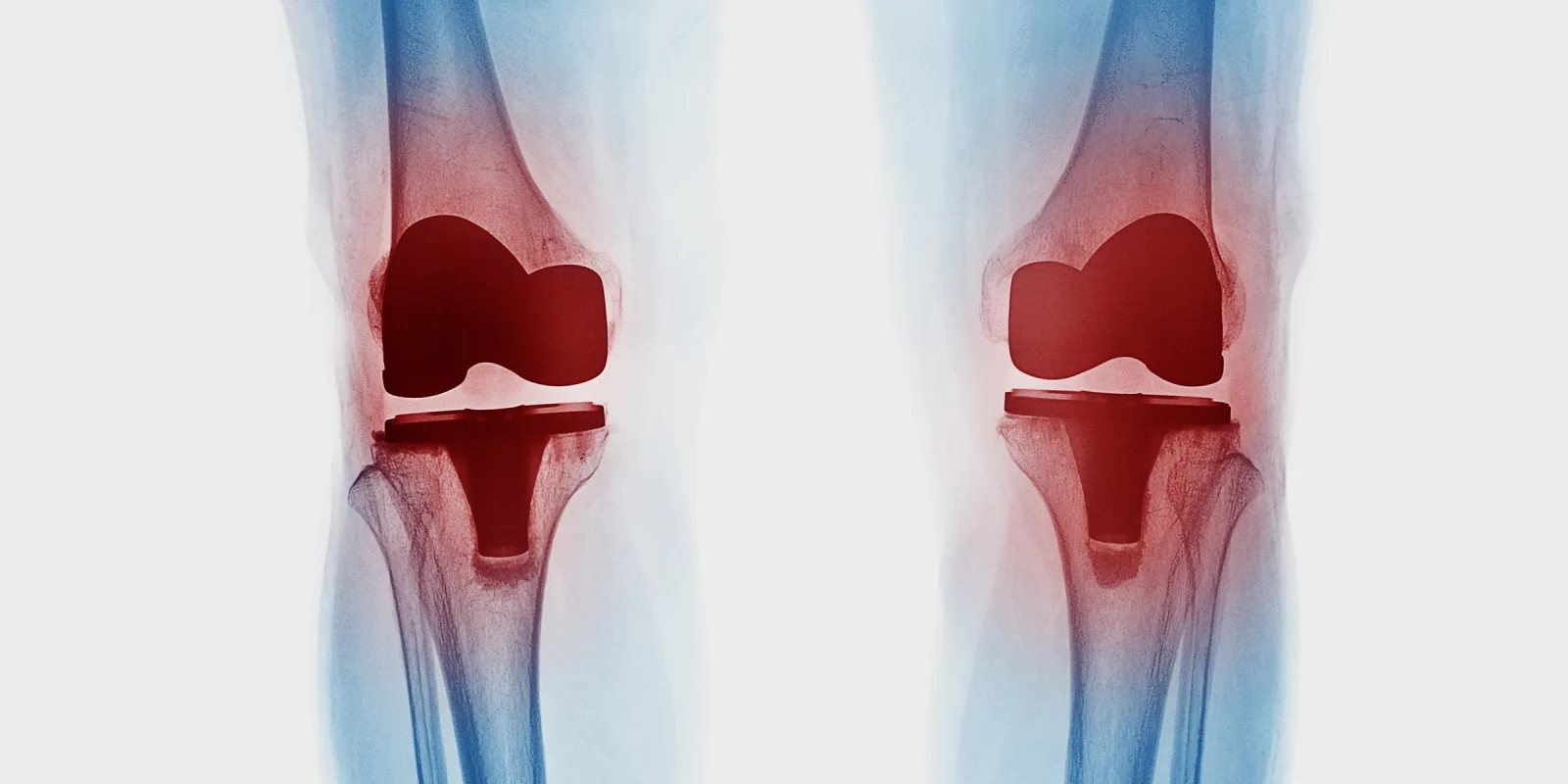
Prosthetic joint infection (PJI) is a dreaded complication of hip, knee, and shoulder arthroplasty that is associated with significant morbidity and mortality. Cefazolin is the preferred drug for preoperative antibiotic prophylaxis in total joint arthroplasty, but in the context of a penicillin allergy, many surgeons use alternative antibiotics. This is true notwithstanding the fact that there is low cross-reactivity between cefazolin and penicillin.
In a recent study, Wu et al. examined the risk of periprosthetic joint infection in patients with penicillin allergies. After controlling for other risk factors, the findings showed that patients with a self-reported penicillin allergy had higher rates of PJI within one year of total knee arthroplasty and total shoulder arthroplasty, but not within one year of total hip arthroplasty.
These findings have important implications for the use of prophylactic antibiotics during arthroplasty surgeries. Allergies to medications and other substances are often self-reported and difficult to corroborate retrospectively with testing or a physical exam, making them susceptible to misdiagnosis or inaccuracy. Patients can confuse an allergy with an intolerance or a negative side effect, or misremember something they were told as a child. While this is not always the case, the harm in the increased risk of PJI following arthroplasty surgery for those receiving alternative antibiotics demands a closer look in the way penicillin allergies are managed in this population.
For patients with a self-reported penicillin allergy, additional time should be spent prior to surgery to obtain more nuanced information about the reaction, and it should be characterized as specifically as possible. While anaphylaxis and severe reactions are obvious contraindications to penicillin and its derivatives, for patients with mild or unknown side effects, the authors recommend a test dose upon entering the OR before administering a full dose.
Wu et al.’s study demonstrates that altering treatment from the standard of care because of a self-reported drug allergy is not a benign decision, and may increase rates of prosthetic knee and shoulder infections. Exploring the veracity of self-reported penicillin allergies and increasing the rate of cefazolin use in this population may help combat PJI in procedures, which is especially important given that the rate of arthroplasty procedures is increasing as the population ages.
Lisa G. M. Friedman graduated from Case Western Reserve University with a medical degree and a master's degree in bioethics. She is currently the orthopaedic trauma research fellow at Geisinger Medical Center. Her interests include shoulder and trauma surgery, and she enjoys creative writing and playing sports in her free time. Dr. Friedman can be found on Twitter, @Shoulder2LeanOn. She is a 2020–2021 Doximity Research Review Fellow.