There was nothing that went according to plan in Mr. Smith’s valve replacement. Every step of the procedure was a struggle, some anticipated and most not anticipated, but we got the valve in place. The procedure had taken a lot longer than expected.
I un-scrubbed and went to meet the family. As expected, they were anxious and nervous and I reassured them, but I did mention the unanticipated complexity of the procedure. I went back into the OR, sat down to finish my report, and heard a shout from inside. I glanced up at the monitor screen, and I saw that the patient was in cardiac arrest — his heart was in a fast rhythm called ventricular tachycardia.
We went right into the resuscitation protocol — shock and external cardiac compressions. The goal of CPR is to provide enough blood flow and thereby oxygen supply to your vital organs. We had the whole team in the room in minutes, but the ventricular tachycardia seemed to effortlessly shrug off everything we threw at it.
My partner started working on trying to get the patient on complete cardiopulmonary support, a procedure called extracorporeal membrane oxygenation (ECMO). This required insertion of two large cannulas (tubes) into the femoral artery and vein, which wasn’t easy given that Mr. Smith was a large man, and there were ongoing chest compressions and intermittent shocking.
I lost count of the number of shocks and drug interventions we had done. We were already 30 minutes into the resuscitation, with no breakthrough. I handed over the resuscitation to my anesthesia colleague and went to talk to the family. It was a difficult conversation to say the least, and the plan was to give it another 10 minutes. By the time I got back things had deteriorated. We couldn’t maintain the oxygen levels anymore, and the blood was becoming more acidotic, reflecting the lack of blood flow and death of tissue.
“I think we should call it,” I said. My anesthesia colleague and everyone else in the room concurred, except my colleague, who was still trying to get the ECMO going.
“Give me a few more minutes,” he said.
Ten minutes later, we got the cannulas in place and got the machine, which serves as a heart and lung, started. It was way too late, I thought, as we gave one more attempt at shocking the patient. But to my surprise, it worked and the patient came back to a regular rhythm.
While conventional CPR clearly saves lives, the outcomes remain dismal. Out-of-hospital survival for cardiac arrests ranges from 2% to 15%, while in-hospital cardiac arrests fare slightly better at approximately 25%. It’s a complex group with survival based on the underlying condition, age, cause of cardiac arrest, and whether there is what we call a rhythm that can be shocked. If the rhythm is not shockable, the prognosis is exponentially worse.
One of the reasons for this poor outcome is that conventional CPR, even with optimal technique, can only generate 25% of normal heart function, which can sustain survival only for a limited time. This has led researchers to look into extracorporeal CPR, or E-CPR, which can not only provide 60% to 80% of normal heart function, but also support entire lung function, buying vital time to fix the underlying problem.
The ECMO circuit is remarkably simple and consists of a centrifugal pump and a membrane oxygenator. Blood is removed through a cannula in a large vein, passed through the oxygenator by the pump, and returned to the body through a cannula in the artery. While the rationale is simple, current research is a mixed bag.
An initial trial out of University of Minnesota, aptly named “ARREST,” generated a lot of excitement with dramatic findings in out of hospital cardiac arrest, with a 43% survival in the E-CPR group versus 7% in the conventional CPR group. The neurological outcomes were even more stunning, 43% in the ECMO arm versus 0% in the standard CPR arm.
Unfortunately, recent larger studies out of the Netherlands and Czech Republic did not show a statistically significant difference between the two methods. The current American Heart Association recommendations conclude that there is insufficient evidence to use E-CPR routinely, but it can be considered for selective patients, where it can be rapidly implemented by skilled clinicians.
The odds were against Mr. Smith — he was much older (84) than most of the patients in the trials and had too many existing medical issues — but to my amazement, he was responding to commands within six hours. Over the next two days, he was weaned off the ECMO and was off all support and neurologically intact. He was discharged to an assisted facility for rehabilitation two weeks later.
While not ready for prime time, all the experts agree that certain patients will benefit from E-CPR, especially the younger patient with an easily reversible form of cardiac arrest. The ECMO devices are getting smaller and more portable. We now also have temporary artificial heart pumps (Impella) that can add to heart support, and when used together, this type of resuscitation is called ECPella.
I can envision the future being a coordinated approach with EMS and the cardiology departments to deliver this therapy in a quick and efficient way to try and improve the survival of our communities. The first steps have already been taken, and we have many miles to go.
*Disclaimer: Patient's name was changed to protect identity.
Dr. Arab is Director of Interventional and Structural Cardiology at AdventHealth, Daytona Beach and Clinical Assistant Professor of Medicine at Florida State University. His passions include triathlon, mountain climbing, and writing.
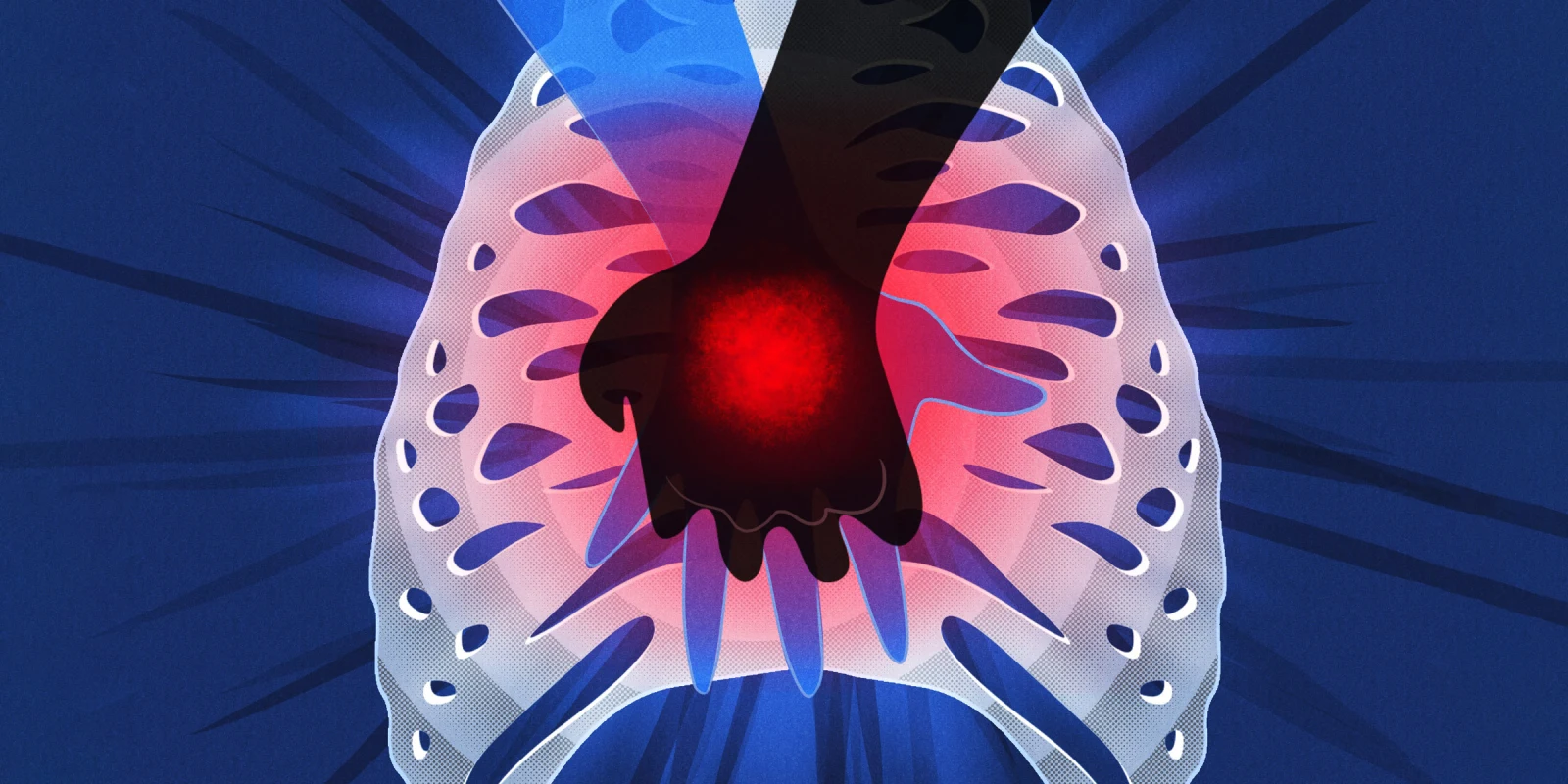
Illustration by April Brust