Dr. Zhen Gooi is a 2020–2021 Doximity Research Review Fellow. Nothing in this article is intended nor implied to constitute professional medical advice or endorsement. The views expressed in this article are those of the author and do not necessarily reflect the views/position of Doximity.
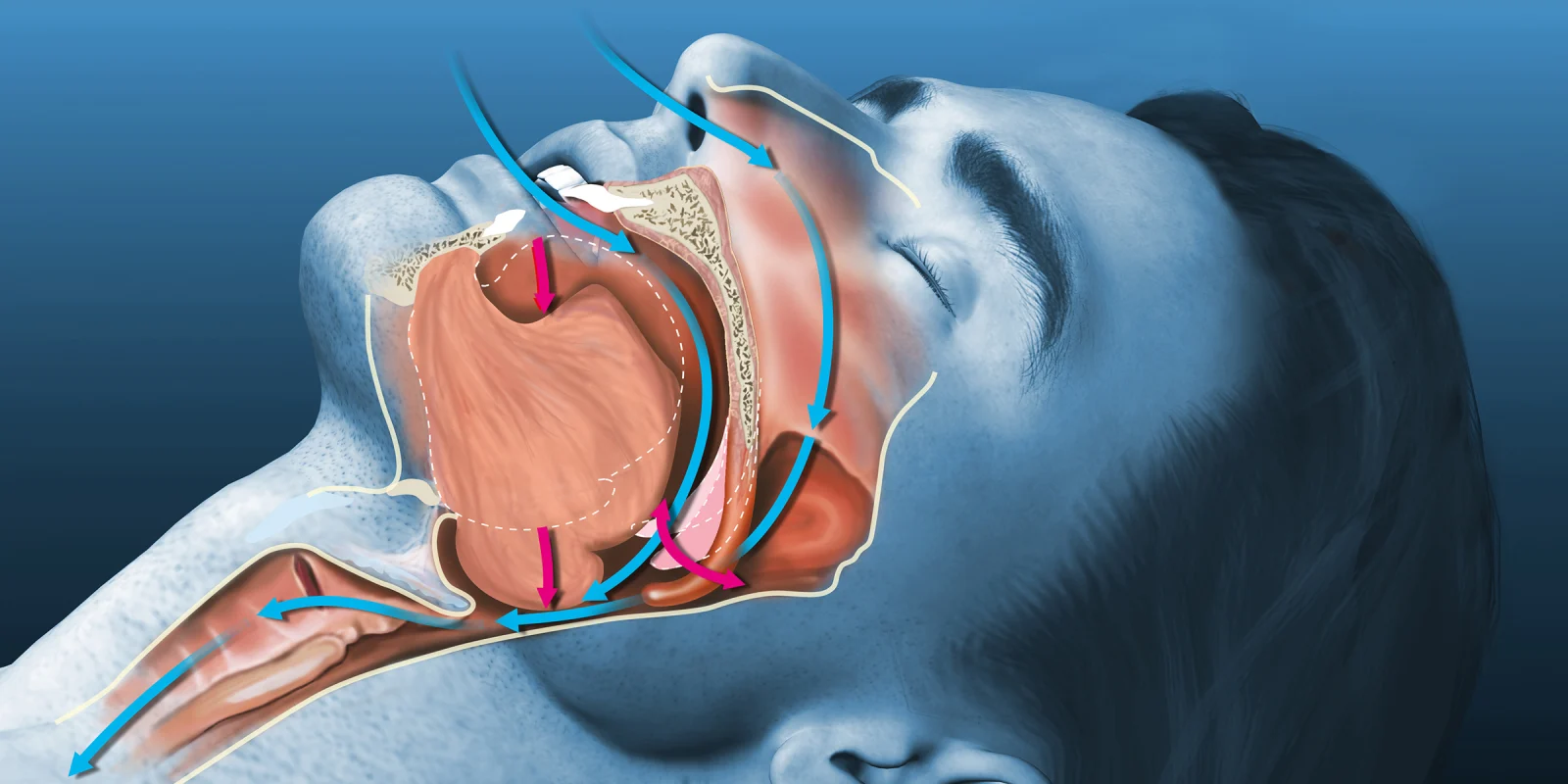
Obstructive sleep apnea (OSA) is a common but also under-diagnosed problem in the general population. While CPAP is considered first-line therapy for OSA, many patients do not tolerate its use or fail to utilize it consistently. There exist a multitude of surgical options to address airway obstruction, but data in support of such interventions has been derived primarily from small, retrospective studies without control or comparison groups.
In a recent randomized trial of adult patients with moderate to severe OSA who did not tolerate CPAP or oral appliance, the effect of multilevel sleep surgery was compared with non-medical interventions. Patients in the surgical intervention group received uvulopalatopharyngoplasty and radiofrequency ablation of the tongue base. Medical management included weight loss management, alcohol reduction, sleep postural modification, and pharmacologic treatment of nasal obstruction.
From baseline to six months, patients in the surgical group had significantly greater improvement in apnea hypopnea index (AHI) (47.9 to 20.8 events per hour) as compared to the medical intervention group (45.3 to 34.5 events per hour). A higher proportion of patients in the surgery group also had resolution of AHI to <10 compared to the medical management group (26% versus 8%). Further, Epworth Sleepiness Scale (ESS) scores were reduced from 12.4 to 5.3 in the surgery group versus 11.5 to 10.5 in the medical management group.
In terms of strengths and weaknesses, the “real-world” inclusion criteria is the former. OSA is more common in men and older adults, particularly in individuals with obesity; here, most of the trial subjects were middle-aged men with obesity. In terms of weaknesses, while surgery resulted in AHI improvement, 57% of patients still had moderate to severe OSA on follow-up polysomnography evaluation. It is unclear whether formal assessment of the pattern of airway collapse was conducted in patients prior to enrollment in the trial. It is also not possible to rule out some element of the placebo effect in ESS score improvement. Finally, the trial did not consider newer therapies (such as hypoglossal nerve stimulation), which would certainly be of comparative interest for future studies.
Dr. Zhen Gooi is a head and neck oncologic surgeon in academic practice at the University of Chicago. He completed his residency and fellowship training at Johns Hopkins University.
Image by Axel_Kock / Shutterstock