“Guys, are you alright in there?” I asked casually, taking the first bite of my dinner on a 24-hour prenatal intensive care unit (PICU) shift.
No answer.
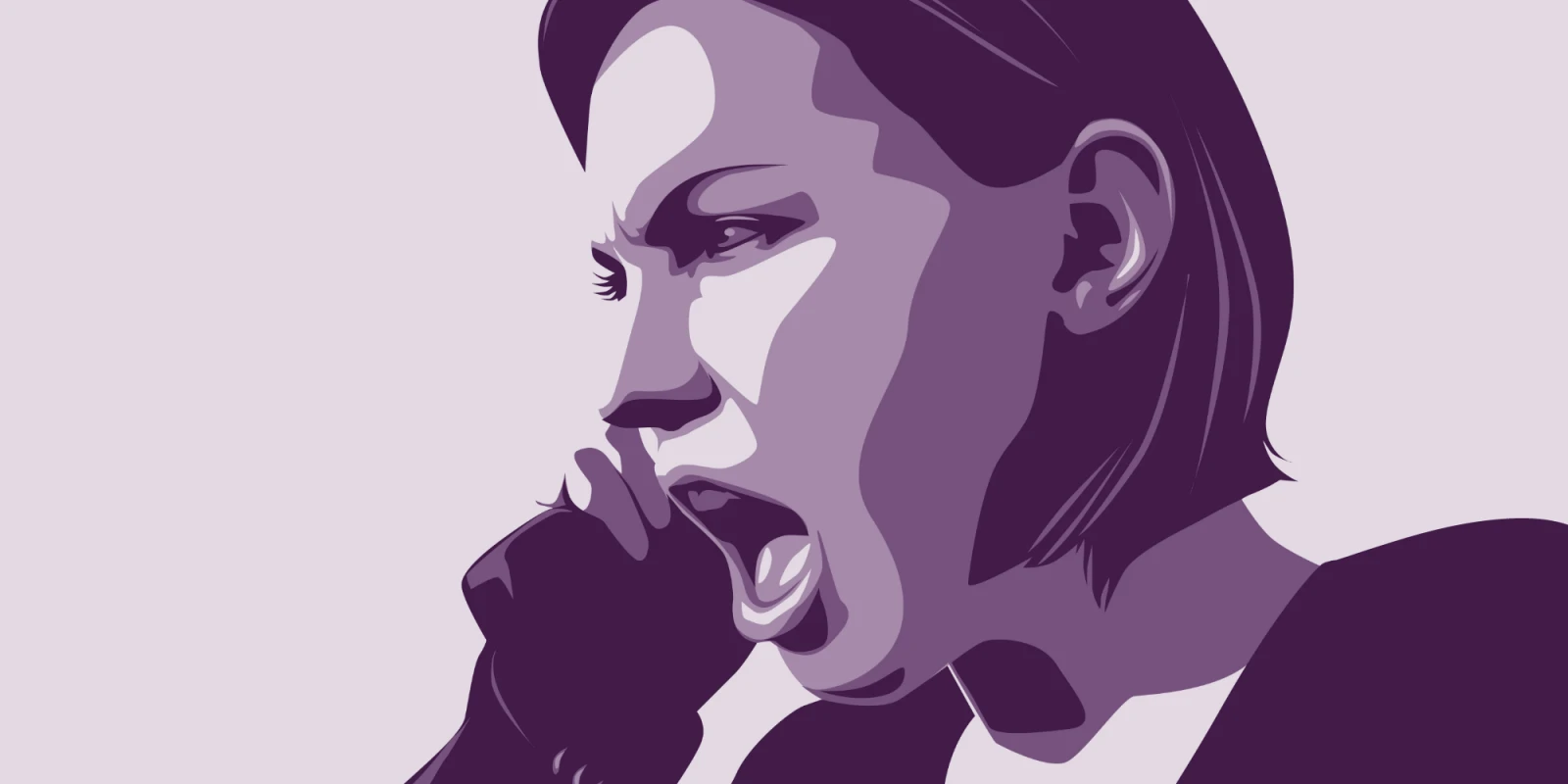
“What’s going on? Why is she beeping so much? Is her tube blocked?” My voice was getting louder.
Complete human silence … except for the deafening hypoxia monitor going to 30s, heart rate monitor dipping to 50s. All of this beeping coming from a 6-month-old girl with a history of brain malformation who was intubated for seizures. I rushed to the patient’s room and quickly realized that she was cyanotic, and not breathing. I started sweating. I could barely keep my hands to myself — I wanted to do everything, but all the things I wanted to do were already being done by someone else. I caught my breath. I approached the respiratory therapist. “What is going on, man?”
“I don’t know. I was just re-taping her tube and it came out.”
Those words echoed in my ears. I noticed the patient’s heart rate persistently below 60. My heart rate was probably soaring above 160.
“Okay, everyone. We are in a code situation. Call the anesthesia attending to the PICU STAT. Call the trauma surgeon STAT. Ask the PICU attending to turn the car around. This patient might need a critical airway real soon. Nurse, I want you on the chest compressions. RT, you are on airway with bag mask ventilation.” My code voice rang out.
Five minutes later, we had a PICU attending, a trauma attending, and an anesthesia attending. All of them had failed to re-intubate. As a lowly second-year resident, I knew if they couldn’t, I didn’t stand a chance to put the tube in. In her code voice, the PICU attending assigned me a role: call the parents, update them about the situation.
Earlier that day, I remembered that these parents had specifically asked me if they could travel to a different city, 300 miles from the hospital, to look at alternative housing arrangements. I had been the one to reassure them that we would take good care of their daughter. My hands shook while I dialed the number.
Ring ring. Secretly, I hoped she wouldn’t answer. But she did, right away. I introduced myself. Before saying anything further, I peeked into the patient’s room, saw that the trauma surgeon was preparing for a tracheostomy tube placement, while the anesthesia resident continued chest compressions for persistent bradycardia.
“I am calling to let you know that your daughter is dying. Right now, we are trying to put the tube back in directly through her neck so that she can breathe. We are compressing her chest to keep her heart beating. There is a high chance that she will not make it tonight.”
Silence. Uncomfortable silence. Yelling. It’s all a blur. I apologized profusely, explained as much as I could, but I don’t think she heard me.
“I am going to kill that *****!” the father yelled in the background. “She better not be dead when I get there.” The mother hung up.
I rushed to the room, looked at the doctors working hard to save the patient’s life. I realized it was the first time I had ever told a parent that their child was dying, and I’d done it over the phone. A few minutes later, the beeping stopped and the nurse yelled: “Heart rate above 100. Stop the compressions.”
With a glimmer of hope I looked up at the monitor to confirm. The trauma surgeon was still working and I prayed to God: “She better not be dead when they get here.”
The next 15 minutes felt more like a decade. The trauma surgeon finally looked at me, with a wry smile and a twinkle of hope in his eyes. He had been successful, she wasn’t going to die.
A year later, as I sat reflecting, I realized that delivering bad news is part of our profession. You learn how to do it, one way or another. As a physician, you are the leader of a team. You have to be clear and concise, you can’t beat around the bush or find an easy way out — rest assured, parents and relatives do not want to hear it. As crude as it may sound, a variation of “dead” sometimes needs to be in the conversation.
That evening, around 11 p.m., I paged my senior resident to bring me some Motrin. And then I interpreted blood gas and electrolyte counts for the patient with diabetic ketoacidosis next door.
This article was previously published on KevinMD.