Several talks at the 2021 SOHO meeting remind us that the treatment landscape of classical Hodgkin’s lymphoma (cHL) continues to evolve rapidly both in the front line setting and in patients with relapsed and refractory disease. Presentations by Dr. Philippe Armand on the first day and Dr. Ann LaCasce and Dr. Steve Ansell on the second provided a detailed and comprehensive overview of the spectrum of new therapies for cHL. In particular, the availability of mature single-agent data allows us to examine the real impact of novel targeted agents, such as brentuximab vedotin (BV) and PD-1 checkpoint inhibitors. Efforts are focused on integrating novel therapies into old backbones or new combinations, both in relapsed patients (transplant eligible and ineligible) and the front line for patients with high-risk diseases.
As reviewed by both Dr. Philippe Armand and Dr. Stephen Ansell, more than a decade of data on the immunobiology of cHL have provided the foundations for the remarkable success of immune checkpoint blockade (ICB). Hodgkin’s lymphoma serves a paradigm for cancer-associated impaired immunity, and the importance of the tumor microenvironment (TME) is exemplified by its classification (nodular sclerosis, lymphocyte depleted, mixed cellularity), which is based on differences in the composition of the microenvironment niche. We now have a better understanding of the cellular and molecular basis of the immune defect in cHL. Hodgkin-Reed-Sternberg (HRS) cells, which only represent 1–2% of the tumor tissue, play a major role in the organization of the TME milieu and protect themselves from immune attack. Loss of expression of MHC class I molecules on HRS cells eliminates an essential docking site for antigen recognition by cytotoxic T-cells (CTLs), and overexpression of the immune checkpoint molecule PD-L1 inhibits effector cell function by engaging PD-1 on the membrane of CTLs. Finally, HRS cells not only influence the function of the immune infiltrate but also the spatial distribution of the different cell subsets, producing a highly specialized biological niche that provides pro-survival signals to HRS and protects them from anti-tumor responses.
It is now clear that the clinical impact of this biology is high. Clinical trials with several different PD-1 inhibitors show that roughly 65–85% of patients with cHL who fail front line ABVD-based chemotherapy and the second-line brentuximab vedotin (BV) respond to ICB. Except for Tislelizumab, reported to have a CR rate of 63% in a Phase II study (N=70), data with Nivolumab, Pembrolizumab, Sintilimab, and Camrelizumab are very consistent: 15–35% of patients achieves CR, a significant fraction (~40%) of which have very durable responses. Most patients, however, progress within two years and require additional therapy. One intriguing observation is that disease progression after PD-1 inhibitors often follows an indolent course. Together with the phenomenon of pseudo-progressions, this has led to the concept of “treatment beyond progression” (TBP). While the evidence is so far limited to retrospective data, there is a signal that patients may benefit from TBP, both in terms of time to next treatment (TTNT) and progression-free survival (PFS). In terms of predictive biomarkers, data from Dr. Shipp’s laboratory show that anti-PD-1 therapy is most effective in patients with a diverse peripheral blood CD4+ T-cell repertoire and abundant activated NK cells, most striking in complete responders. One last practice point discussed by all speakers is that prior treatment with ICB may sensitize cHL chemotherapy. Limited but intriguing data show higher than predicted response rates to chemotherapy post-ICB in patients with heavily pre-treated cHL, with CR rates up to 40% and remarkably durable PFS.
In her discussion, on day two, on how to integrate novel agents, Dr. Ann LaCasce provided a comprehensive clinical overview of BV and ICB, and in particular ongoing efforts to combine and compare these two new standards of therapy in cHL. In the frontline setting, for patients with advanced-stage cHL, the 5-year update of the ECHELON-1 study, just published, show a continued advantage in PFS for the BV-AVD arm with no changes in toxicity. However, in the subset analysis, the advantage seems to be most evident in PET2-negative younger (younger than 60) patients, suggesting BV-AVD may not be the answer to the unmet need of older patients with high-risk diseases. If not BV-AVD, then what? Supported by limited but very encouraging Phase II data with sequential ICB-chemotherapy combinations in patients with untreated cHL, a randomized Phase III trial is now in progress comparing BV-AVD and Nivo-AVD in patients with advanced-stage disease (NCT03907488). For consolidation therapy, the long-term follow-up data of the AETHERA study, which randomized high-risk cHL patients (primary refractory, response of fewer than 12 months, or extranodal disease) undergoing autologous stem cell therapy (ASCT) to one year of maintenance BV versus placebo, confirm the robust PFS benefit of BV.
In the relapsed setting, Dr. LaCasce discussed several BV-containing salvage chemotherapy regimens that showed remarkable CR rates (70-80%) with 70-80% PFS at two years, suggesting that BV-containing salvage regimens can be considered for BV-naïve patients with relapsed cHL. Mature data (36-months follow-up) are also available for the combination of BV and nivolumab at first relapse. PFS was 77% after four cycles of BV-Nivo, and 91% for those who proceeded to ASCT. Less mature but intriguing, the combination of Pembrolizumab and GDP appears promising in a small (N=37) study with one-year follow-up, with 95% CR rate and all patients proceeding to ASCT.
Several studies incorporating BV and chemotherapy in the front-line setting in patients with early-stage disease, bulky and non-bulky, have been completed. Results are encouraging, in particular suggesting that radiation therapy may be avoided in PET-negative patients. A similar strategy, using nivolumab instead of BV in patients with untreated early unfavorable and advanced stage, shows encouraging response and PFS data. Follow up is short for all these studies, however, and these combinations will have to be tested in randomized clinical trials before being embraced as new standards.
Dr. Porcu is employed by Thomas Jefferson University and has received consulting fees from Daiichi, Viracta, and Innate Pharma
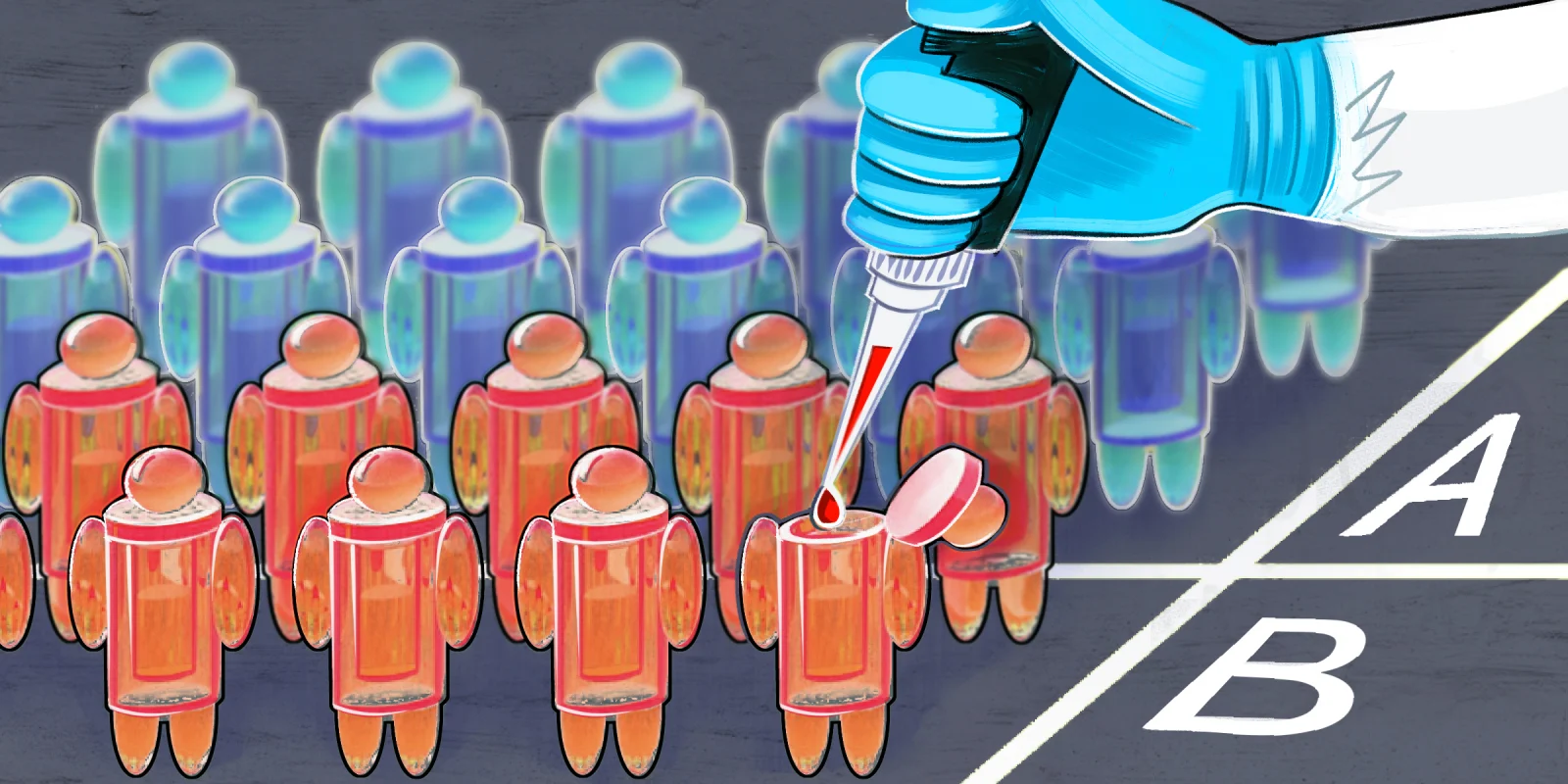
Illustration by April Brust