Technological advancements in anesthesia care have paved the way for remarkable innovations that enhance patient safety, precision, and efficiency. To name a few:
- Ultrasound-guided regional anesthesia that greatly enhances precision of local anesthetic delivery while minimizing iatrogenic tissue and organ damage
- Bispectral index monitoring that non-invasively analyzes brainwave patterns and evaluates level of consciousness
- Target-controlled infusion systems that maintain precise circulating drug concentrations
- Robot-assisted anesthesia devices that enhance procedural precision and drug administration
These examples and several others indicate the utility of technology in anesthesia provision. Whether via elevating access to relevant and timely information, enhancing precision of procedures and drug delivery, or improving patient safety with advanced monitors, technology is here to stay and its utility grows further still.
The use of technology, however, is not without significant limitations.
When it comes to medical technology, “new” is almost synonymous with “expensive.” The acquisition of cutting-edge equipment, software upgrades, and ongoing training initiatives may not be within financial reach of all health care facilities, thus limiting access to a select group of users.
Technical malfunctions and system failures can potentially compromise patient care. The interconnected nature of electronic systems raises concerns about data security and patient confidentiality. While technology is viewed as “helpful,” there is growing trepidation of “over-reliance” and the loss of human skills. The learning curve associated with transitions into newer technology may initially disrupt efficiency and be faced with resistive inertia.
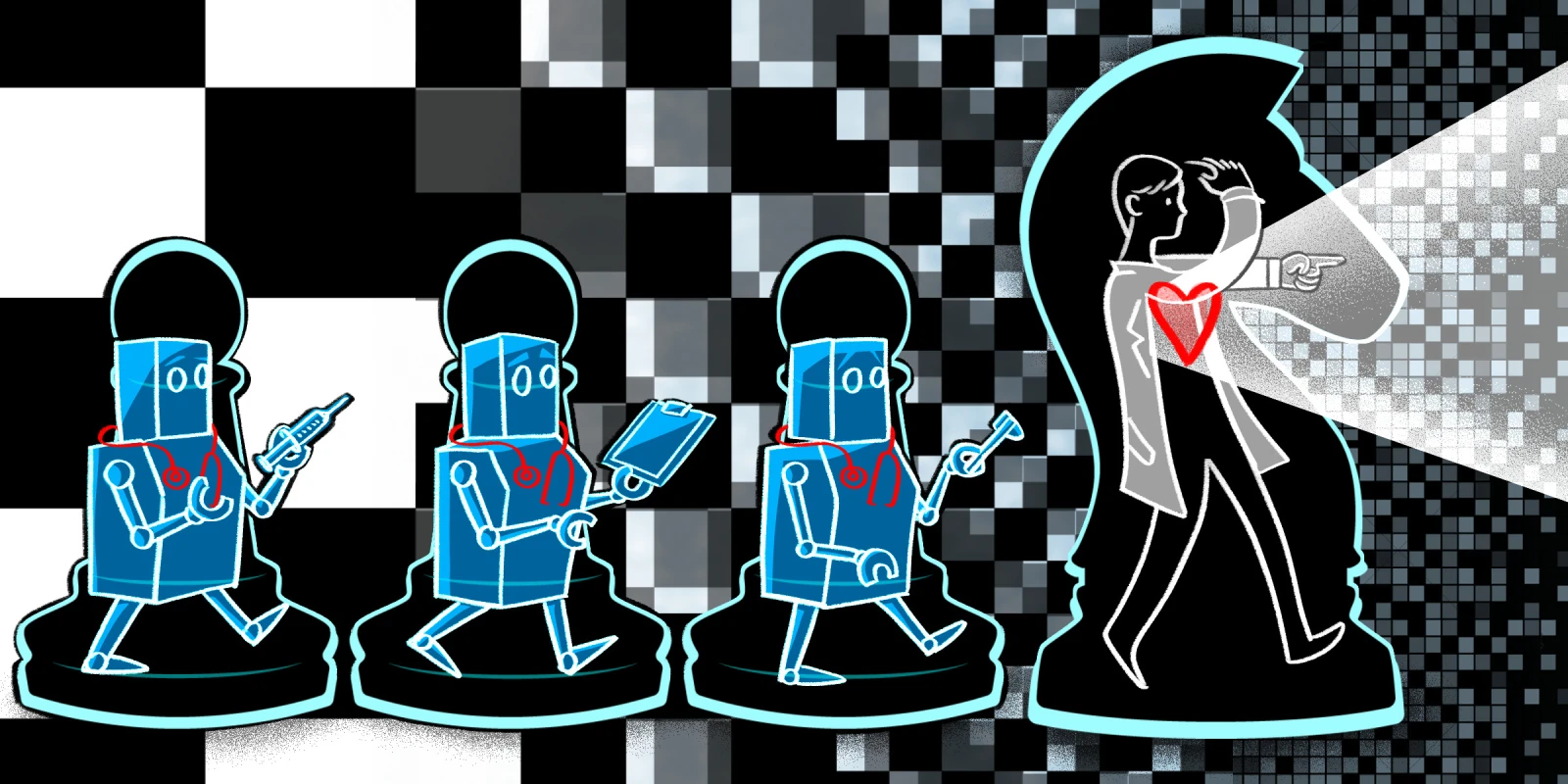
Another important facet to discuss is job security. The incorporation of technology into the practice of anesthesia has raised concerns among anesthesiologists. This takes shape in the multiple ways technology has been and is planned to be assimilated into everyday anesthesia practice. Automating tasks — monitoring, drug delivery, and feedback loops — is one of the more pronounced arguments typically presented that may, on the surface, seem to detract the need for anesthesia providers. This has been seen in other departments such as hospital pharmacies, where automation seems to add value to managers and higher-level staff while devaluing the role of technicians.
Automation has, in fact, been shown to save hundreds of thousands of dollars annually by enhancing error detection and optimizing anesthesia billing. The picture is less clear when it comes to clinical duties, especially those involving direct patient contact. Nevertheless, the practice of anesthesia goes far beyond a job that could be automated. Anesthesia providers are tasked with the complex responsibility of assimilating monitor prompts into reasonable, biologically plausible, and situationally correct scenarios where different interventions can mean life or death. In that sense, allowing some automation in anesthesia practice may be quite beneficial. A vital signs monitor that would predict a drop in blood pressure or oxygen saturation based on trends or another monitor that would combine data from multiple inputs to indicate the level of consciousness can readily find much value in the busy and complex process of administering anesthesia. The anesthesia provider could then reserve more time and attention to other tasks such as maintaining proper documentation, closely following the surgical procedure, or educating trainees.
And then there is the fact that these technologies remain in constant need of leaders who understand their use and can direct their development. Those leaders and innovators are the ones to develop new skills and elevate their clinical and technological acumen to meet the demands of the fast-paced world of medicine we are all experiencing. Combine that with the inherent need for collaboration in anesthesia, coordination with other medical teams, and the value of the essential “human touch” in anesthetic practice, and you’ve got yourself a field that can only adapt and evolve. It was no coincidence that anesthesia was responsible for some of the most dramatic increases in patient safety practices in medicine, and there is no reason to believe we couldn’t continue with that legacy.
Do you think automations will help or hurt medicine? Share in the comments.
Dr. Saasouh completed an anesthesiology residency at the American University of Beirut (Lebanon), a research fellowship at the Cleveland Clinic Department of Outcomes Research (Ohio), where he was chief research fellow, received training in neuroanesthesiology at the Cleveland Clinic (Ohio), and completed an anesthesiology residency at the Detroit Medical Center (DMC-Michigan). He is currently a Board-certified Anesthesiologist and a Director of Research. Dr. Saasouh was a 2019–2020 Doximity Conference Fellow, a 2022–2023 Doximity Op-Med Fellow, and a 2023 Doximity Digital Health Fellow.
Illustration by April Brust