Willie’s attentive demeanor toward Anna never wavered. He attended every one of her prenatal visits and all of her prenatal classes. He was perhaps 19, maybe 20. In spite of his young age, his devotion to the mother of their baby was noteworthy. Despite my numerous attempts to engage him in conversation, he remained aloof and reticent, altogether stoic, never rude. As an obstetrician, I always made it a priority to get to know my patient’s significant other, the one who would be there during labor to support my patient and help guide her through the painful contractions that would surely come.
When Anna’s prenatal visits became more frequent toward the end of the second trimester, it became obvious Willie and I failed to connect. I tried sports. I questioned him about his family, his interests, his work. Attempts at humor fell flat. Nothing pierced the veil that enveloped him. Anna was white, Willie was Black. Never succumbing to the temptation to ignore him, I finally retreated to the conclusion Willie probably tolerated me, a white male, only because I was Anna’s obstetrician and had cared for her since she was in high school, when she came in for her first annual exam and initiated birth control.
Once Anna’s membranes ruptured, her labor progressed normally without incident. After each exam, I shared my findings and thoughts with the two of them, along with explanations about the laboring process. When asked if he had any questions, Willie remained mute. Late in stage 2 labor, the fetal heart tones sustained a prolonged deceleration that failed to recover at the conclusion of the contraction. I briefly explained my concerns, and Anna consented to an assisted vaginal delivery. Willie’s apprehension intensified when he saw the unwrapped forceps. Avoiding the sound of bringing the forcep blades together, I confirmed they articulated properly and explained the procedure while reassuring Anna and Willie there was little risk.
One last exam confirmed the baby’s presentation. After successful placement of the forceps and a single pull, a seemingly healthy baby boy emerged. Willie severed the umbilical cord and the nurse scooped the baby up, showed him to Anna and Willie, then attended to him in the warmer. While finishing up a laceration repair and thinking ahead to the delivery note I’d have to write, I looked over at the nurse and said, “Apgar’s eight and nine?”
Most everyone knows what an Apgar score is, or has at least heard of it. Virginia Apgar, an anesthesiologist, first introduced the scoring system in the 1950s in an attempt to standardize and score a newborn’s condition. Virtually every newborn delivered in the last six decades in the U.S. has been provided an Apgar score. Its five components are heart rate, muscle tone, skin color, reflex, and respiratory effort. Each component is assigned a score of 0, 1, or 2 at both one minute and five minutes of life. Occasionally, if necessary, a score at 10 minutes is provided. A score of eight or above is reassuring. Seven is marginal and a score of six or less is suggestive of a problem.
I was cutting the last knot on the repair when the nurse responded, “Six and eight.”
Somewhat surprised, I said, “Six?”
“Yeah, the initial heart rate was down just a bit and his reflexes were poor. Plus, I took two off for color.” The nurse then held the baby up for all to see on her way to Anna’s side.
Now I had heard “two off for color” any number of times in any number of settings, but never had I heard it or thought of it in a racial context. However, it was the first time Willie had heard it, and all he heard was “two off for color” from his son’s first examination.
Willie stood as straight as an iron stake and demanded to know what his baby’s color had to do with anything. I replaced the placenta back into the basin before its inspection was completed and engaged his stare. I explained what an Apgar score was and what “two off for color” meant and emphasized it had absolutely nothing to do with his race — that it was simply a way to assess his son’s early oxygenation status, nothing more.
Willie’s posture immediately softened. I don’t know if it was my explanation. It probably had more to do with seeing his son snuggled up to Anna’s breast. Whatever the reason, he leaned down and studied his son. He stroked the smooth skin of his son’s cheek and said, “I can’t believe how small his fingernails are.”
Anna looked up and smiled, “Look, he’s got your nose.”
Willie looked at me and nodded. His nod confirmed he understood what the nurse had meant. It was then I knew Willie and I had finally connected. And it was at that moment I began to understand something I had never before contemplated.
Over the ensuing years, my recollection of Anna’s delivery has never diminished. As I reflect upon the turmoil and events in this country these past two years, I feel certain Virginia Apgar, in 1958, never envisioned the racial implications of partially scoring a newborn based upon its color — but perhaps she should have. Was she a racist? Probably not, and that’s beyond the point. Moving forward, we should always consider the potential impact of our words and actions upon others and not just in a racial context. Rather than relying on the simplicity of the Golden Rule, we should actively and intentionally consider our words and actions upon others and temper them accordingly. In doing so, the vast majority of slights and insults would altogether be avoided.
Have you had patient encounters that helped you understand their perspective? Share your experiences in the comment section.
Lloyd Holm is a retired obstetrician who lives in Cottage Grove, Minnesota with his wife, Gretchen. He has authored two novels and a children’s book and his writings have appeared in the Omaha World Herald, The Female Patient, Iowa Medicine, Contemporary OB/GYN, Hospital Drive, the American Journal of Obstetrics and Gynecology, and Obstetrics and Gynecology. While a member of the teaching faculty at the University of Nebraska Medical Center in Omaha, he received the Dean's Award for Excellence in Clinical Education and The Hirschmann Golden Apple Award. Dr. Holm is a 2021–2022 Doximity Op-Med Fellow.
All names and identifying information have been modified to protect patient privacy.
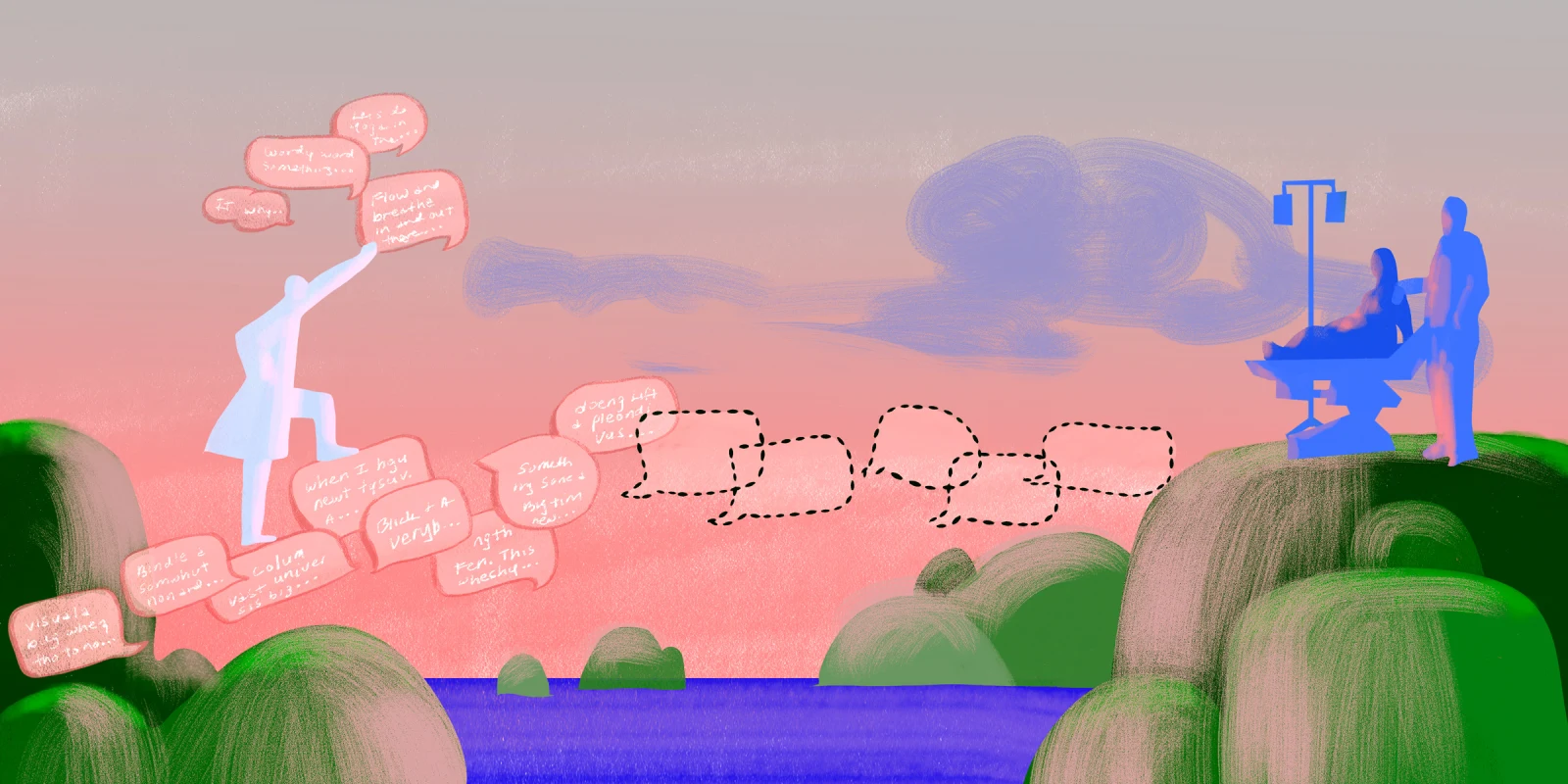
Illustration by Jennifer Bogartz