Stress and burnout have multiple effects. Over half of current medical practitioners now report at least one feature of burnout, which may include emotional exhaustion and numbness, feeling robotic or mechanical, and a low sense of personal accomplishment. While the medical community has become aware of the ubiquity of this issue, the conversation often stops at the effects of physician burnout and stress on physicians themselves. Although this is of course a vital conversation, our well-being and function matter not just for our own health but also for optimal treatment outcomes and patient safety — which is why we must simultaneously discuss the effect our impairment may be having on our patients.
Whether we’re aware of it or not, our physical and mental status (and our patients’ perceptions of it) affects not only how we communicate with patients, but also how they receive our guidance. As just one example, our level of empathy with patients is linked to the degree of stress and burnout we are experiencing. Clinicians with burnout may be more likely to stigmatize their patients with negative stereotypes; this is true even of psychiatrists.
Additionally, studies have shown that patients interpret our demeanor, physical appearance, and work pace as indications of our health. This, in turn, affects how much they trust us and how much they adhere to our recommendations. Patients often understand that we are affected by our work, and may, in response, offer reassurance and answer health questions optimistically, rather than accurately and realistically. They may also limit the number of problems they disclose to us during a session, thereby reducing our ability to diagnose and prescribe accurately.
Further, even if patients don’t pick up on it, clinician work stress has been linked to several care issues: decreased professionalism, individual medical errors, and poorer team performance. Similarly, physicians experiencing burnout make more diagnostic, clinical reasoning, and therapeutic mistakes than our more satisfied colleagues. And depressed residents make more than six times as many medication errors as their non-depressed peers. Given that stress, burnout, and more serious physical and mental problems erode the quality of empathy and care we provide, it is imperative that we seek and follow methods to improve, then sustain, our well-being.
Fortunately, these methods may not be as inaccessible as we think. Professional stress has been shown to be lower in practitioners who devote time to hobbies, are in a partnered relationship, and who spread their vacation time throughout the year. Practicing playfulness is also a useful way to reduce stress and increase adaptive coping strategies to counter it. Studies have shown that play and recreation boost resiliency and enhance teamwork, creativity, adult academic achievement, and emotional and intellectual strength. The effort to engage in playful acts is more important than the nature of the activity; you should choose something that you enjoy and that will maintain your interest. Barring these approaches, time itself may offer a salve — research has found that stress is more common among practitioners with fewer years of clinical experience.
Clinician burnout can also be treated and mitigated. One way to do so is by claiming and obtaining greater control over how we work, choosing how, when, and where our responsibilities are discharged. Whenever possible, vary your work, dividing it, for example, among direct patient care, consultation, research, and teaching. How we approach these clinical efforts can also matter: set and communicate boundaries regarding time, and between work, home, and social life. Balancing work with the rest of our responsibilities is an essential skill that we can develop as our careers progress. Maintaining these professional boundaries is also necessary for optimal clinical reasoning and practice. We need to become more aware of our own mental health needs and be willing to seek help. Thinking about our own feelings will help increase our empathy and tolerance as we increase our understanding of the diversity of human cognition, behavior, and experience.
In addition, we can diminish our burnout experience via mindfulness and other metacognitive techniques, which allow us to exercise cognitive flexibility in our clinical reasoning. Further, as clinicians we have the power to not only prescribe, but also to utilize stress management, personal coaching, and cognitive behavioral therapy to increase our own communication and coping mechanisms. If you are a supervisor or administrator, allow your clinicians a greater role in decision-making, decreasing job demands while increasing their control over their work. Structural steps you can take to help them include alterations of schedules and reevaluation of methods, work flow, and practice environments.
Colleague, peer, and outside support are also key for maintaining our well-being and optimal performance. It is important that we be attuned to our coworkers and prepared to not only seek, but also offer, support. The opportunity to safely and bidirectionally share doubts and errors with others, without fear of repercussion, is invaluable. We can also utilize our professional association resources, such as these from the American Medical Association and others from our specialty organizations. Opportunities to meet with colleagues in a semi-professional setting will broaden our perspectives, increase feedback and information, and allow more time for reflection on our skills and practice.
As clinicians, we have an ethical imperative to present ourselves in a healthy and optimally functional state when we offer to help patients. To accept the responsibility of their care while in any degree of impairment is an abdication of our commitment to and therapeutic alliance with them. With the variety of wellness steps available for us to utilize (e.g., mindfulness, play, cognitive behavioral techniques, stress management, yoga nidra, mutual peer support, and healthy personal and professional boundaries), we can reduce the effect that stress, burnout, and more serious health problems have on treatment outcomes. As clinicians serious about quality care, we must first look to ourselves.
What stress management techniques do you utilize? Share in the comments!
Dr. Putman is the author of Rational Psychopharmacology: A Book of Clinical Skills and Encountering Treatment Resistance: Solutions Through Reconceptualization. He blogs at drpaulputman.com. Dr. Putman is a 2024–2025 Doximity Op-Med Fellow.
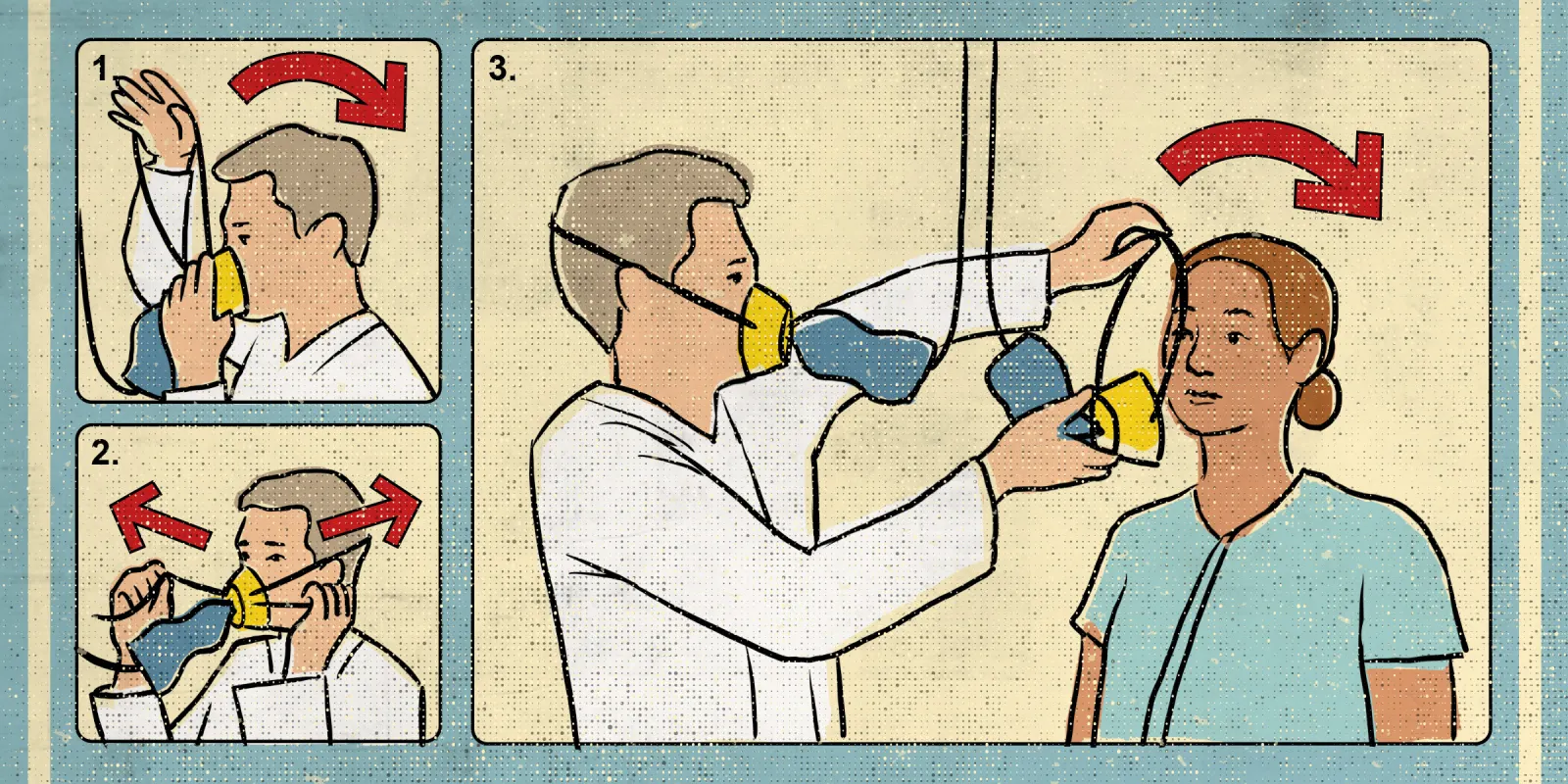
Illustration by Diana Connolly