A group of researchers that questioned why more than 30 years later HIV-1 diagnosis is still a challenge for many hospitals has figured out a way to make it easier for more patients to be tested.
While the CDC has repeatedly recommended screening for HIV-1 for patients in all healthcare settings, many hospitals have not followed the recommendations. In 2006, for instance, the CDC issued a recommendation stating that “HIV screening is recommended for patients in all health-care settings after the patient is notified that testing will be performed unless the patient declines (opt-out screening).”
There are many barriers that prevent hospitals and clinicians from acting on the opt-out screening recommendation. For starters, it can be an expensive program for hospitals to run. Another barrier is hospital-based clinician reluctance since some may think there isn’t enough HIV in their population to justify the costs of looking for the disease. Others cite low-positive predictive value for screening, or insufficient linkage to proper care.
“One of the other major reasons that people don’t do HIV screenings is that at these hospitals who do screening, the patient has to come back a second day for more definitive testing,” said Dr. Kathleen G. Beavis, Medical Director of the microbiology and immunology laboratories at the University of Chicago Medical Center. “We saw that as a barrier, to have people come back, so we figured out a way that with the additional tube of blood if they are positive on the screening we could do multiple testing from that one tube of blood.”
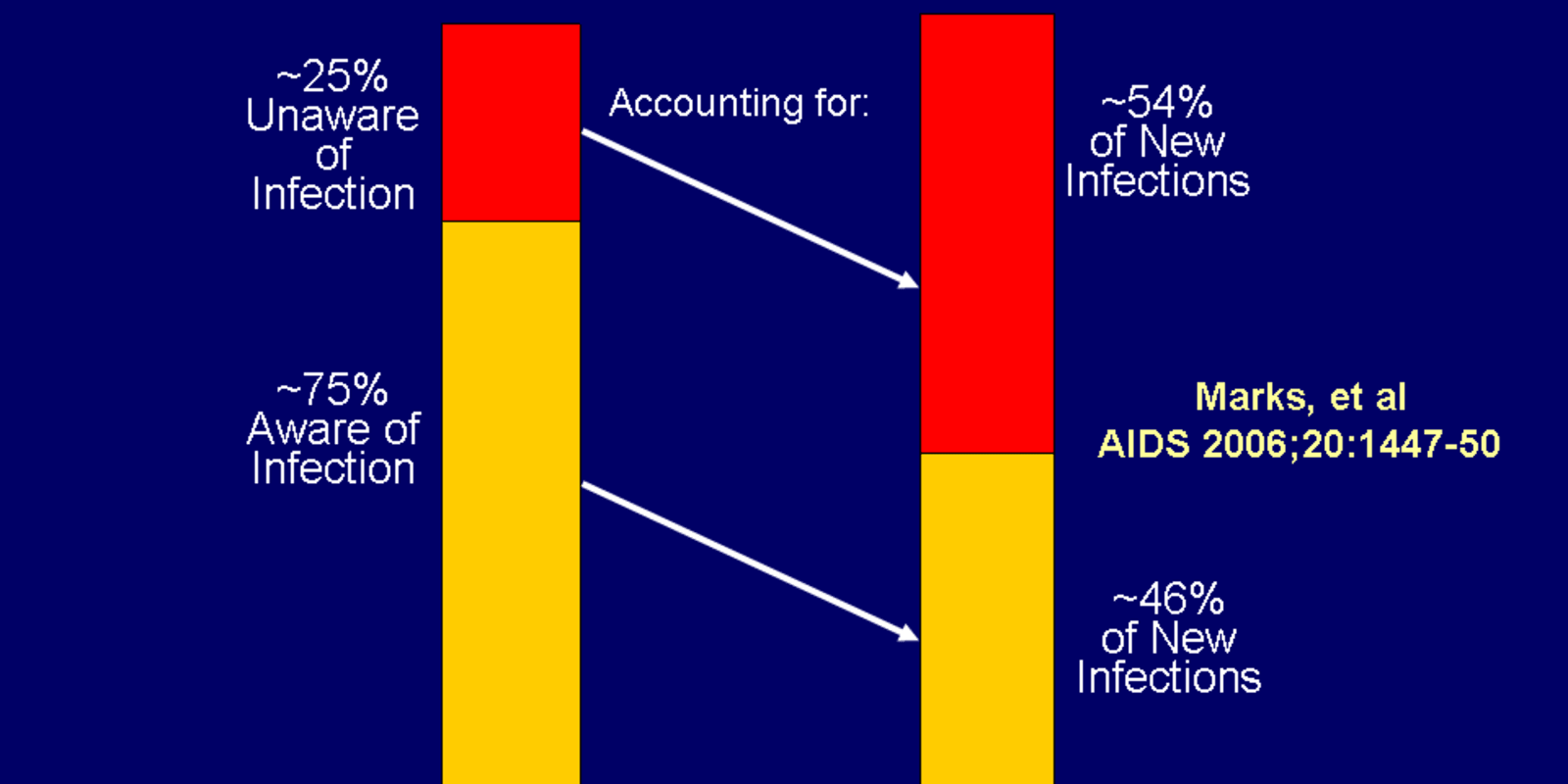
Beavis is the lead author of the research that aims to streamline HIV diagnosis, which was recently presented at ASM Microbe 2018. She cited CDC findings that many people still live without knowing that they have HIV, and these people are transmitting HIV when they have sex, share needles, or engage in other behaviors.
“There is a lot of research, however, that proves that individuals who are aware that they have HIV are more likely to change their behavior (i.e. sexual practices, hygiene habits) to reduce the risk of transmission,” explained Beavis. “We’re changing laboratory practices by streamingling the diagnosis — allowing from diagnosis to viral load to be made from a single of tube of blood instead of having the patient come back for additional testing.”

Going forward, the researchers are working on education to reduce some of the barriers to diagnosis. At ASM Microbe 2018, they discovered that many hospitals or healthcare systems of attendees were not following CDC recommendations.
“We had a lot of people come up to us afterward and ask for our help, giving their input,” said Beavis, “since they’ve been trying to do the screening at their institution, but have been running up against a lot of roadblocks.”