Cushing’s syndrome, primarily caused by hypercortisolemia, has recently gained public attention following the announcement by actress and comedian Amy Schumer in February 2024 that she has been diagnosed with the condition. This spotlight on Cushing’s syndrome, while bringing necessary awareness, also underscores the importance of understanding its intricate aftermath, particularly the challenges faced by patients even after successful treatment.
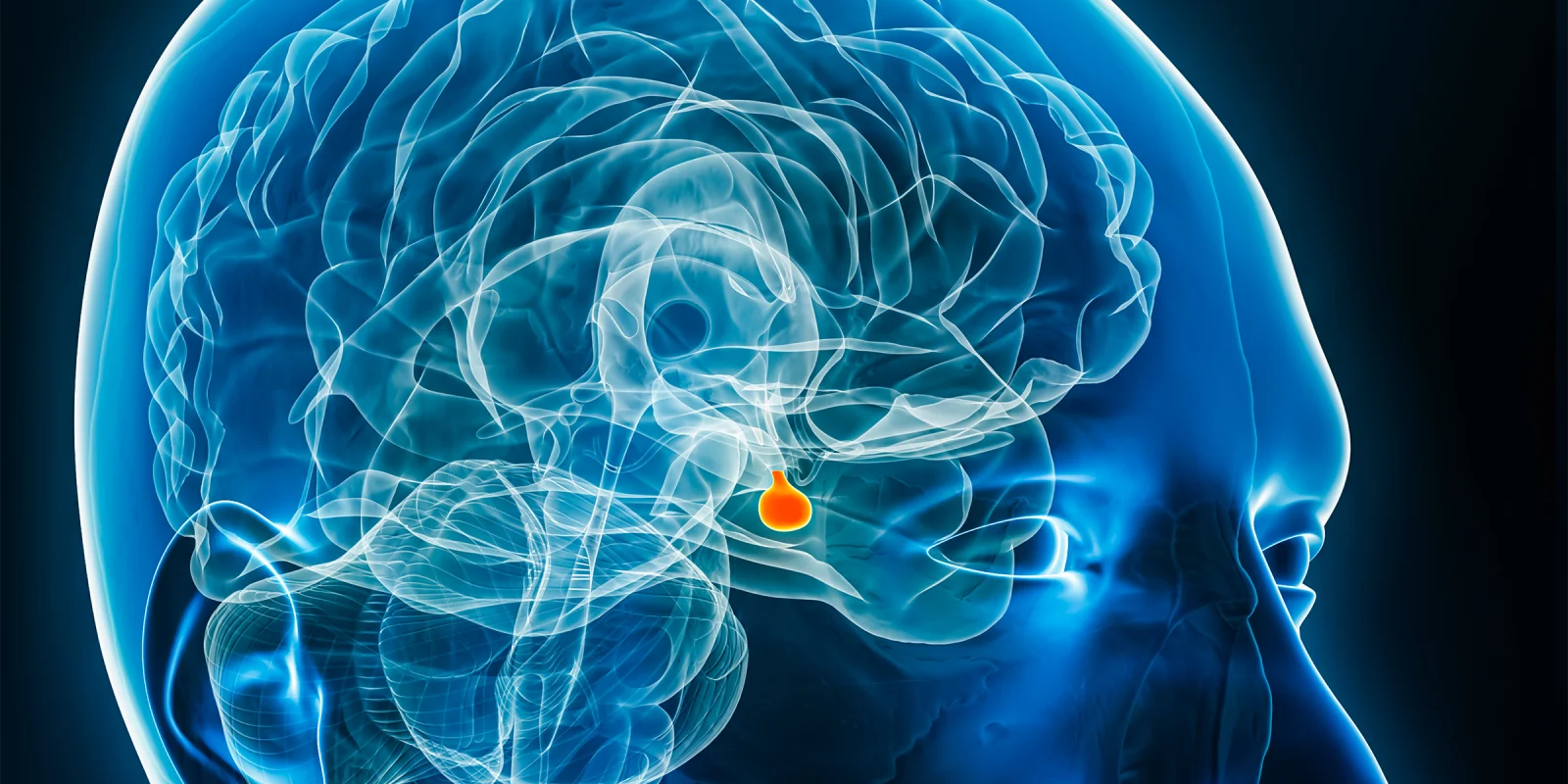
Cushing’s syndrome due to endogenous hypercortisolemia is rare, with an incidence rate of approximately one to two cases per million people annually. This rarity often complicates both the evaluation and management of the disease. Among the various forms of Cushing’s syndrome, Cushing’s disease, specifically caused by a pituitary adenoma that overproduces adrenocorticotropic hormone, is a significant subset. The standard treatment for Cushing’s disease is the transsphenoidal resection of the pituitary tumor. While this surgical intervention is generally successful in inducing remission, the journey to full recovery is fraught with challenges.
Patients who undergo successful tumor removal face a prolonged and difficult recovery period that can extend beyond a year. This post-surgical phase is marked by a constellation of symptoms which significantly affect the quality of life. Moreover, individuals exposed to long-term high-dose glucocorticoids for other conditions experience similar symptoms, collectively known as glucocorticoid withdrawal syndrome. Despite advancements in surgical techniques and medical management, the precise mechanisms driving these post-Cushing’s syndrome symptoms remain elusive, and effective management strategies are not well-defined.
The recent ENDO2024 symposium, held on June 2, shed light on this critical issue through a dedicated session on recovery following the remission of hypercortisolism. One of the notable talks was delivered by Dr. Grethe Astrom Ueland, who discussed the role of inflammatory markers in Cushing's syndrome before and after treatment. Her research identified Fibroblast Growth Factor 21 (FGF-21) as a key biomarker, providing new insights into the inflammatory processes involved in the syndrome.
Dr. Lisa Nachtigall, in her presentation, highlighted the increased incidence of inflammatory diseases following the cure of Cushing's disease. Her findings indicate that the inflammatory response does not simply resolve with the normalization of cortisol levels but may persist or even intensify, complicating the recovery process.
Another significant contribution came from Dr. Catherine Zhang, who presented her study on managing glucocorticoid withdrawal syndrome. She proposed a structured glucocorticoid initiation and tapering regimen to mitigate withdrawal symptoms. Dr. Zhang’s findings provide a practical framework for clinicians to follow, aiming to reduce the discomfort and health risks associated with abrupt cessation of glucocorticoids.
Despite these advancements, there is a consensus among experts that further research is essential to fully understand the underlying mechanisms of post-Cushing's disease symptoms and to develop comprehensive management strategies. The discussions at ENDO2024 represent a promising start, bringing together leading minds in endocrinology to address the unmet needs of patients struggling with the aftermath of Cushing’s syndrome and glucocorticoid withdrawal.
The personal stories of individuals like Amy Schumer bring a human face to these clinical challenges, fostering empathy and encouraging a broader conversation about the complexities of Cushing’s syndrome. As research progresses and new treatment protocols are developed, there is hope that the recovery process for Cushing’s syndrome patients will become more manageable, ultimately improving their quality of life.
In conclusion, the overlooked aftermath of Cushing’s syndrome is a significant issue that extends beyond the initial treatment phase. The prolonged recovery period, marked by persistent and debilitating symptoms, underscores the need for continued research and refined management strategies. The insights shared at ENDO2024 are a step in the right direction, offering hope and new perspectives for patients and health care providers.
Dr. Min has received a grant for a phase 3 trial.
Image by libre de droit / Getty Images