Edwin Rowan was born in Ireland. He was the boxing champion of his weight class at 14 years old, and was my grandfather. He was diagnosed with metastatic melanoma when I was beginning my third year of medical school — stepping foot into clinical medicine for the first time in my new white coat. While my cohort was learning about brain tumors and anti-epileptics and steroids on our neurology rotation, I was thinking about my grandfather who had already started a concoction of these medications, which he took religiously every day.
Even with his medications and cancer therapies, he continued to get worse. My grandfather was the first person I saw who was postictal, the first person in whom I saw Todd’s paralysis. I knew that, during my third year of medical school, I would start to see patients embody the disease processes we had been learning about in classrooms for the past two years, but I didn’t expect my grandfather to be one of them. I didn’t expect my grandfather’s oncologist to pull me aside while my grandfather was hospitalized after a seizure and fall to show me his brain scans and worsening tumors — treating me like I was a medical student and not a granddaughter.
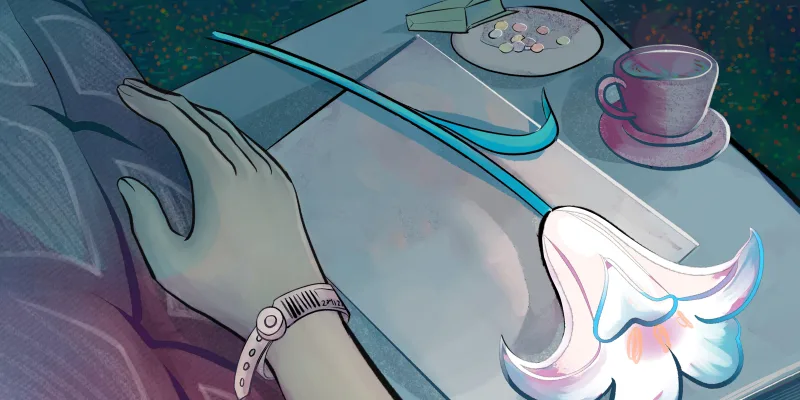
My grandfather hadn’t wanted to die in a hospital, connected to IV tubing or a mechanical ventilator. He had wanted instead to die in his home. He passed away only months after his diagnosis, during the early Florida spring. I remember the long days with my parents and home hospice nurse, surrounded by the new additions to my grandfather’s home — hospital bed, morphine, and pamphlets on hospice care describing the symptoms of an actively dying person. I remember the moments where I sat next to him as he lay dying, watching the morning sunlight stream into his bedroom. In those moments, we were filled with sorrow and grief and yet somehow enveloped with peace, somehow brought closer together. My grandfather wasn’t in pain; he was surrounded by those he loved, spending his last days in the home he cherished, a home he had shared with my grandmother for so many years until her death only a few years prior in the very same room.
This sense of stillness yet togetherness — grief complemented by peace and finality — is a feeling I’ve experienced only a few times since. As a third-year emergency medicine resident, I have now pronounced deaths many times — calling time of death after long, traumatic codes in the ER or ICU. I don’t often experience the feeling after these types of codes, as many of these deaths are unexpected and decidedly not peaceful — but every once in a while, I do feel it, usually when the patient does not want resuscitation and is surrounded by loved ones. It is a spiritual subdued experience shared amongst the family with myself as a proxy. I am allowed into this private moment — a moment of trust — because of my job. This feeling is present in the still moments, as I listen to the deceased patient's silent heart and lungs and feel for a non-existent pulse, before I quietly tell the family what they already know — their loved one is gone.
I’ve found witnessing deaths in the ICU to be worse than in the ER. I see the families of the patients every day, get to know the children and siblings and partners. My patient’s daughter showed me and my co-resident a photograph of her father attending her wedding only days before he had his heart attack. He looked so alive in his tuxedo, smiling with his family. So different from the intubated man lying in the ICU bed behind us.
I used to feel self-conscious about showing sadness and sharing grief with patients and their families. When I would feel a swell of emotions inside me, I would attempt to harden my heart and bury the emotion deep down — afraid that expressing sadness in front of a patient and their family would be looked down upon, would be selfish, would make me a bad doctor. As a defense mechanism, I would avoid certain patients’ rooms unless I truly had to go in, knowing that seeing the patient and their family would deepen our connection and make it that much worse if they died.
But by turning away from these emotional moments surrounding death — whether it be because of the fear of being in pain or being perceived as weak — we miss opportunities for deep connection and intimacy. We miss opportunities to turn toward each other instead of away, to lean into crying in front of a patient and their family, sharing in their grief. These moments have the chance to bring us closer together, like my family did through my grandfather’s process of dying. These moments are when I have felt the most human.
Being vulnerable to connection, even if it might also bring along pain, will make us more open as people first and make us better doctors second. After all, these sacred moments are ultimately the reason many of us entered medicine in the first place. And these are the moments that matter the most.
Have you encountered the process of death and dying in a medical setting? Share your experience in the comment section.
Dr. Halloran is an emergency medicine physician currently completing residency in Chicago. She works and writes at the intersection of health policy, inequality, and education, and her research and writing has been featured by the American College of Emergency Physicians and by Slate. She can be found on Twitter at @Diana_Halloran. Dr. Halloran was a 2022-2023 Doximity Op-Med Fellow.
Illustration by April Brust