The treatment of shoulder instability in athletes is continually advancing. Previously, open Bankart reconstruction of the shoulder yielded positive outcomes for both high-level and recreational athletes. However, despite its success, open surgery posed risks such as stiffness, loss of function, and potential osteoarthritis. These challenges paved the way for arthroscopic management of shoulder instability, which promised to address underlying issues while reducing the morbidity associated with open procedures. Arthroscopy significantly minimized the risks of infection, neurovascular injury, and postoperative adhesions, with initial studies suggesting outcomes comparable to traditional open approaches.
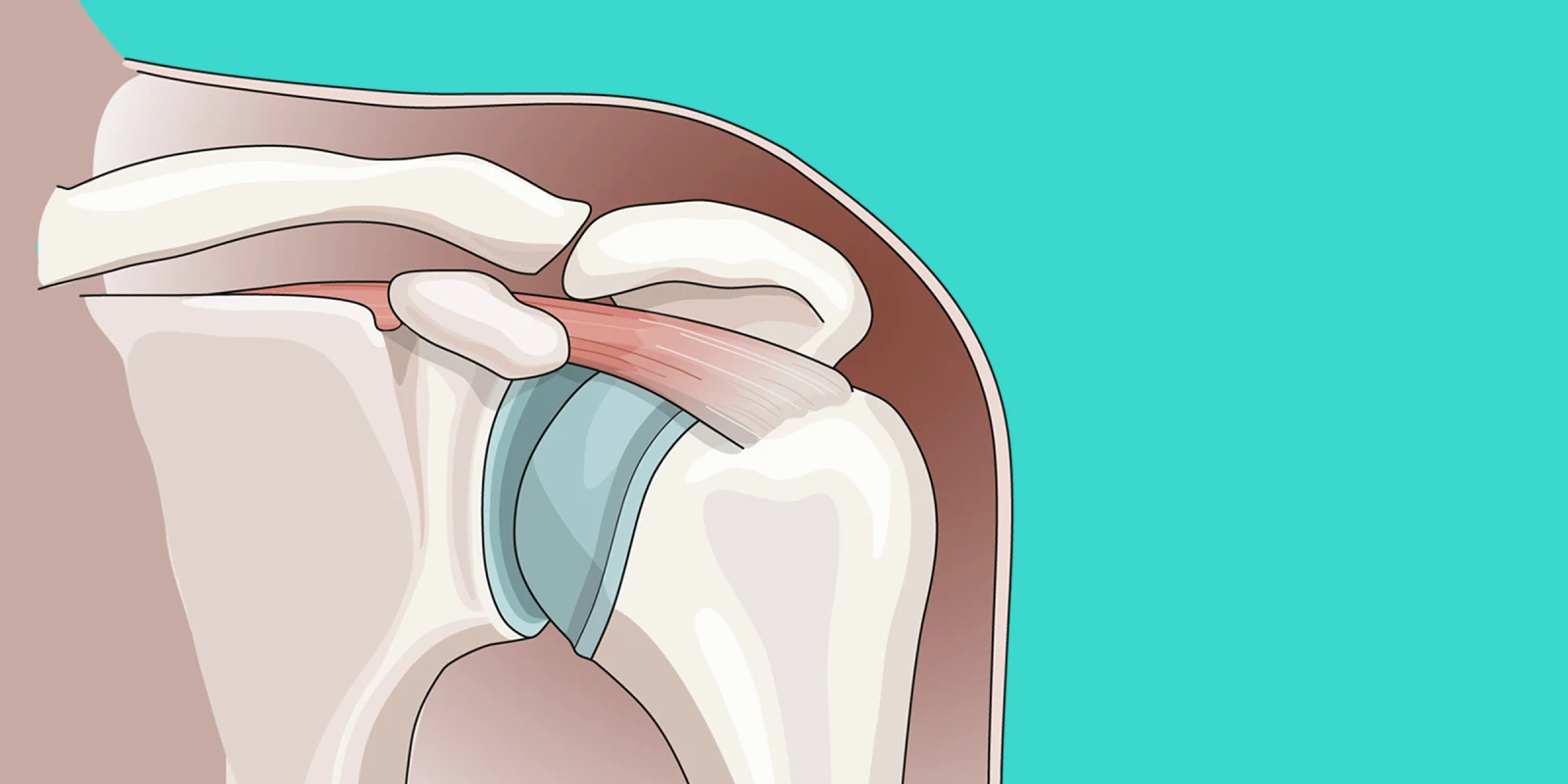
However, upon closer examination, it became evident that the risk of recurrence and the ability to return to sports were not as optimized as initially thought, particularly in high-level athletes. This patient population presented unique challenges, as the demands on the glenohumeral joint often exceeded the capabilities of soft tissue fixation provided by open or arthroscopic Bankart repair alone. Consequently, many contact or collision athletes experienced failures, sometimes resulting in structural changes to the glenoid or humeral head that placed increased stress on the labrum soft tissue repair.
To address these issues, some European practitioners began employing open bone grafting procedures, such as the Bristow/Latarjet reconstruction, as a primary intervention in younger patients with shoulder instability. However, concerns regarding neurovascular injury, postoperative stiffness, and the risk of osteoarthritis have limited the widespread adoption of this technique in the U.S.
In line with the ongoing evolution of treatment techniques, newer approaches combining bone grafting with arthroscopic methods have emerged, generating considerable interest within the orthopaedic community. These advancements were showcased at the recent American Academy of Orthopaedic Surgeons Annual Meeting in San Francisco, CA, particularly during the AOSSM/ASES specialty day program. Notably, Dr. Ivan Wong presented his refined technique of arthroscopic distal tibia allograft reconstruction, along with promising results from a substantial patient series involving glenoid and humeral head bone defects. Additionally, Dr. Robert Arciero, a distinguished figure in the field, shared insights gleaned from his extensive experience caring for athletes with shoulder instability during the Kennedy lecture.
The ongoing pursuit of optimal outcomes in this challenging patient population raises several important questions:
- Is distal tibia the best graft option or are newer graft options (distal radius) going to prove more reliable and available?
- Will the risk of arthritis be reduced with a less invasive and anatomically congruous graft?
- Will artificial intelligence help us in the future to determine the best treatment option for patients with complex instability patterns (open v. arthroscopic Bankart repair, remplissage, open bone graft, etc.)?
As the field continues to evolve, collaborative efforts such as specialty conferences serve to foster innovation and knowledge exchange. It is through platforms like the AAOS meetings that leading experts can convene, share insights, and collectively strive for advancements that benefit patients.
Dr. Fotios Tjoumakaris is an orthopaedic surgeon in Egg Harbor Township, NJ, and is affiliated with multiple hospitals in the area, including AtlantiCare Regional Medical Center and Thomas Jefferson University Hospitals. He received his medical degree from Rutgers Robert Wood Johnson Medical School and has been in practice 17 years. He specializes in elbow surgery, orthopaedic sports medicine, and shoulder surgery and is experienced in osteoarthritis, sports medicine, rotator cuff tears, knee injuries, and knee arthroscopy.
Image by Irina Medvedeva / Getty Images