Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) may have a welcome benefit in addition to weight loss and glycemic control, with new data presented at ObesityWeek, the annual meeting of the Obesity Society, showing that use of these medications is associated with a reduction in problematic alcohol use.
The relationship, observed in a cohort of US military veterans, appeared to be slightly stronger in those with versus without obesity.
There is significant overlap between alcohol use and obesity, said Alissa Chen, MD, an instructor at Yale School of Medicine in New Haven, CT, who presented the findings. They share similar neurologic underpinnings, mostly related to the dopamine reward pathway, and both are influenced by hormones like ghrelin, orexin, and melanocortin that regulate food intake and reinforce drugs of abuse.
In that context, “there’s been quite a buzz about the potential ability for GLP-1 receptor agonists to improve alcohol use,” Dr. Chen said, pointing to preclinical studies showing reduced alcohol intake in mice and an exploratory analysis of a randomized trial suggesting that exenatide decreased heavy drinking days in patients with alcohol use disorder (AUD) and obesity. In addition, a large observational study suggested that the GLP-1 RA semaglutide lowered the incidence and recurrence of AUD compared with other anti-obesity drugs.
This new study explored the issue using data from the US Veterans Health Administration, which covers much of the cost of GLP-1 RAs when used to treat type 2 diabetes and obesity. Among a cohort of more than 2.1 million patients with type 2 diabetes (mean age 68 years; 95% male) who received care in fiscal years 2017 to 2023, 12% received at least one prescription for a GLP-1 RA, most commonly dulaglutide, semaglutide, or tirzepatide (which is also an agonist of the glucose-dependent insulinotropic polypeptide [GIP] receptor). Those who received a GLP-1 RA were more likely to be obese (BMI ≥30 kg/m2) compared with those who did not (85% vs 63%; P<0.001).
Unhealthy alcohol use was defined using the Alcohol Use Disorders Identification Test (AUDIT-C), which is obtained regularly for every veteran in primary care. Scores range from 0 to 12, with a score ≥3 for women and ≥4 for men indicating alcohol misuse.
Using negative binomial models adjusted for potential confounders, Dr. Chen’s team showed that veterans who were prescribed a GLP-1 RA were less likely to have a 1-point increase in AUDIT-C, both among those with obesity (prevalence rate ratio [PRR] 0.78; 95% CI 0.77-0.78) and those without obesity (PRR 0.81; 95% CI 0.80-0.82).
It is “hard to know if that’s clinically meaningful,” Dr. Chen said about the difference in estimates based on obesity status. “They’re very close. They’re also separate models. But notably those with obesity had a slightly lower prevalence rate ratio, so maybe less alcohol use as compared to those without obesity.”
There are some limitations of the analysis, she acknowledged, pointing to the cross-sectional design and the possibility of unmeasured confounding. In addition, although there is a benefit to having a cohort of mostly men since many GLP-1 RA studies include mostly women, “this is not necessarily generalizable to a population that is not veterans [and] not mainly men and mainly white.”
Nonetheless, Dr. Chen said, this study provides “more supportive evidence to say that there’s something there with GLP’s and alcohol use.”
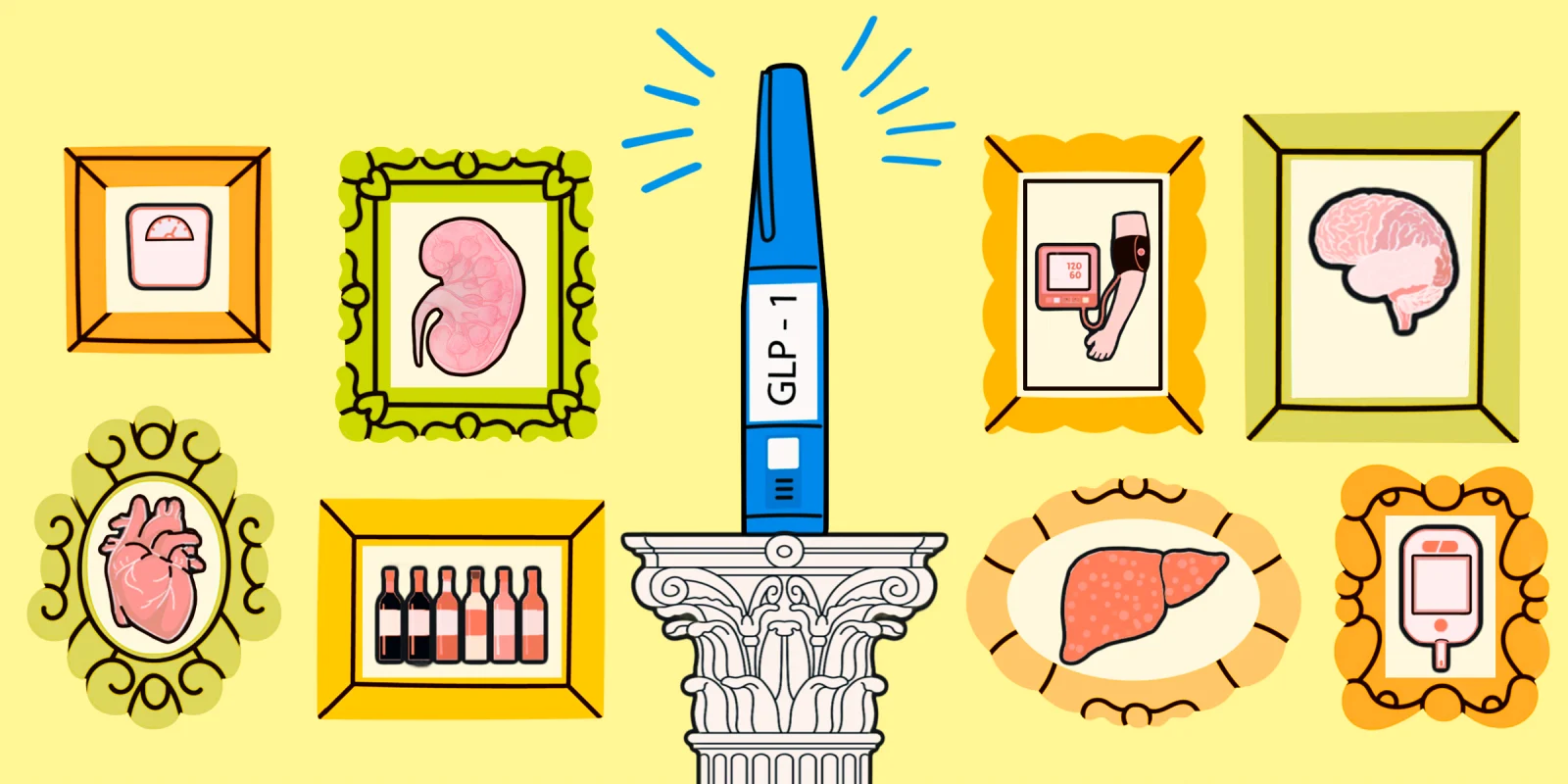
Collage by Jennifer Bogartz / Shutterstock