Patients with severe asthma have increased morbidity, and up to 25% of patients may have four or more exacerbations annually. Effective asthma management requires a personalized approach, including addressing asthma triggers, patients’ education, symptom and lung function monitoring, and pharmacological management. Often, these patients require high-dose inhaled corticosteroids (ICS) and additional controller medications, usually long-acting beta-agonists (LABA). Those who remain uncontrolled despite high-dose ICS/LABA and have type-2 inflammation usually require biologic therapy. Omalizumab was the first biologic agent approved by the FDA in 2003 for patients with moderate to severe persistent allergic asthma aged 12 and above. Since then, several new biologics have been approved and have shown to be very effective and safe in patients with severe asthma. Despite the efficacy and safety profile, prescribers may feel constrained by the prescribing guidelines, health care infrastructure, and financial burdens on the patient. This issue was very eloquently highlighted by Dr. Meredith Turetz during her presentation at CHEST 2022 annual conference in a session, “Ask the Experts: Biologics in Airway Disorders.” She is an Assistant Professor of Pulmonary and Critical Care Medicine at Weill Cornell Medical College.
Dr. Turetz highlighted that biologics are expensive and the health care system is complex with multiple insurance programs, including Medicare, Medicaid, commercial plans, etc. Most of these drugs require prior authorizations and multiple back-and-forth communication with insurance companies and specialty pharmacies, which may lead to delays in access. Insurance providers may also ask to use a biologic agent on their formulary first and may have high-cost sharing tiers that could discourage the use by the patient. A recent study showed that the time from the biologic prescription to the first dose was approximately 44 days. Delays in access to biologics are not without consequences, as 47% of patients in this study required the use of systemic steroids while waiting for biologic therapy.
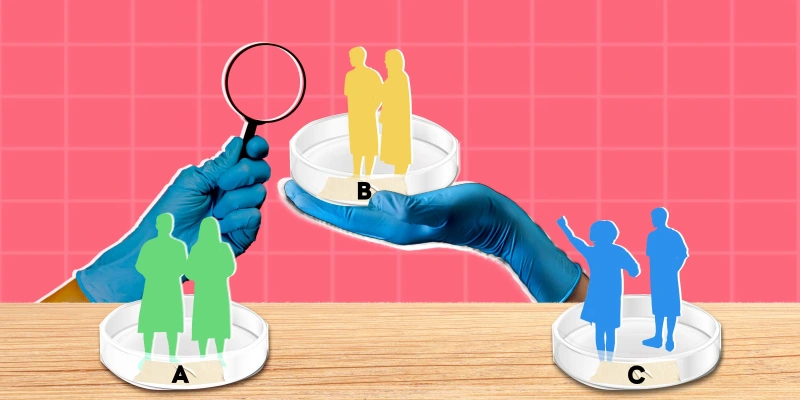
Dr. Turetz also shared the data on disparities in access to biologics in asthma. In an analysis of biologic use in the U.S. from 2003 to 2018, patients with higher income, commercial insurance, and access to a specialist were more likely to use biologics. Similar findings were noted in another study assessing biologic use by payer mix among patients with asthma and showed that biologic treatment visits were higher for those with private insurance (28.3/1000 visits) compared to publicly insured (16.3/1000 visits). The study also noted that among the publicly insured patients, white patients accounted for 80% of the treatment visits despite only accounting for 60% of the asthma visits. Dr. Turetz concluded her talk by emphasizing minimizing delays and addressing disparities in access to biologics for severe asthma patients.
Dr. Adrish is employed by Baylor College of Medicine, and has no conflicts of interest to report.
Image by nadia_bormotova / GettyImages