My home security system is very smart. Our alarm is synchronized to our thermostat, which is also synchronized to our home lighting, and all of these devices geotrack to my phone. In fact, I can set the indoor lights and fans to turn on when I (via my phone) am within 1 mile of my house. Moreover, these various “household departments” communicate with each other when we are on vacation to ensure we do not waste money in our heating/cooling bills and also regulate our lights so that we illuminate our home in a manner that matches our normal lighting patterns in order to signal our presence to all outsiders. Again, I would describe this technology as being smart in that it is well designed and accurately predicts my desired settings as an end user.
However, when I log in to a hospital EMR system, I often experience the opposite: outdated systems that have no idea of my patterns or needs. Multiple times, I must log in to a cumbersome software program that requires excessive clicks and redundant layers of documentation in order to perform a simple task. “Order a chest X-ray?” 8 clicks. “Find the report for yesterday’s chest X-ray?” 18 clicks. This complicated, disjointed end user experience extends well beyond medical records and broadly affects most medical devices. Why is there such a gap between the technology provided at home at virtually no cost and expensive health information systems? Regulation, for one. I do think there is a design flaw that is inherent to these systems: the end user — physicians — are practically absent when the product is developed. Be it a consequence of us being busy or not being invited, we physicians rarely offer meaningful input in the actual design of most software products that are purported for us to inevitably use.
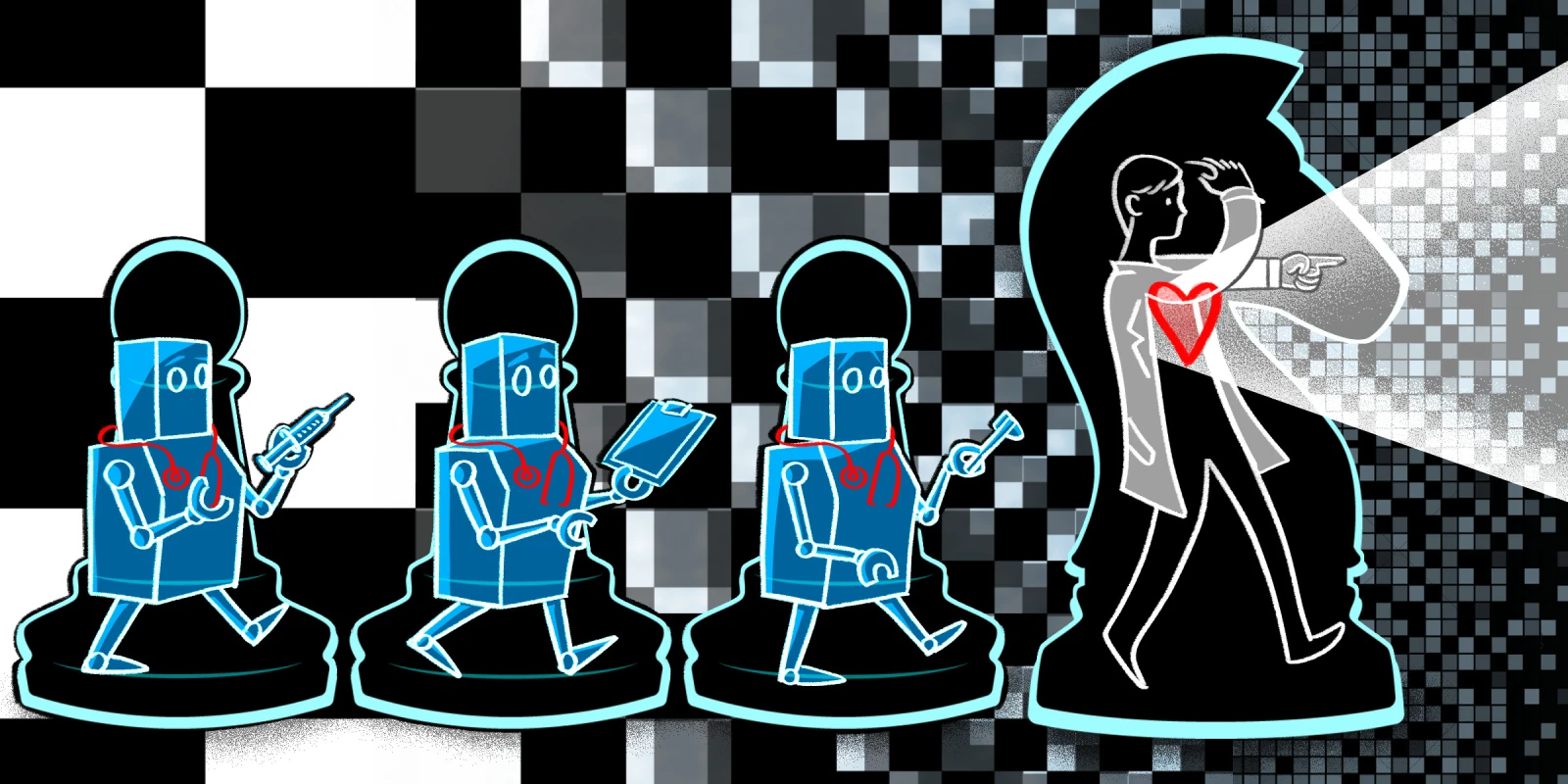
I could easily continue a dissertation about the lack of respect for physician input in the design of health care information systems but that would not offer true insight into the actual disconnect between design and end user needs. I have met with countless software developers and I find them to be incredibly thoughtful and curious individuals who crave any feedback from physicians. In fact, most of the health IT personnel I’ve worked with have job options and take pay cuts or equivalent sacrifices simply because they feel they are contributing to a larger goal, as if they are working toward a calling. If anything, they are extremely motivated to get the product right. They just aren’t clinicians. Ideas and features that sound great to a developer may not be useful in the clinical realm. Moreover, the integration of a new product into an existing health care system can lead to increased complexities in the form of excessive logins, numerous software bridges, and workarounds that ultimately undercut the very efficiency the technology strives to achieve. While this disconnect is frustrating, I worry our general absence in design will have a larger threat. We are approaching a legitimately existential threat in innovation that will force us to re-evaluate our basic offering to patients. Yes, the great disruptor of (medical) decision-making: Machine learning. And we have to get ahead of it.
Most of our value proposition to patients comes in the form of our human capital. We have been extensively trained to ingest data in the form of physical exam findings, lab results, and imaging. We, as doctors, process this data in order to develop a diagnosis and treatment plan, which, combined with our natural empathy and humanity, is our offering to patients in a nutshell. (I realize reducing the entire medical offering to a sentence comes with some generalized error, but humor me.) While this offering is difficult to quantify or replicate, our thinking can be mapped out into a decision-matrix and tested. Our diagnostic approach to renal failure or ARDS may be replicated by cognitive neural networks capable of analyzing countless more data inputs than we can (such as patient ZIP code) and, possibly, yield a more nuanced conclusion than us.
While our decisions currently entail a blend of our experiential knowledge and (immediately) available clinical data, we may be outmatched with an algorithm that can process more inputs and compare them to larger reference sets than our memory. These models have already been deployed to assist in detecting breast cancer on mammograms or predicting which patients will need a C-section and, while are currently deployed in their early iterations, are here to stay in my opinion. As much as we have offered patients to date, too much of our methodology may be equally well performed (and hopefully not outperformed) by machine learning. How do we stay relevant? Immerse ourselves in this space and pivot. Obviously, our empathy and ability to connect with patients and other humans is not to be understated and, likely, another key distinguishing feature that we should continue to harness, if not for empathy’s sake for job security.
Information asymmetry, broadly defined as access to information that is hidden to the public, has been the basis of countless professions: real estate agents, accountants, and taxi drivers, for starters. Over time, ubiquitous internet access and novel technological advancements have disrupted these professions in remarkable fashion. The lay individual has much greater access to high level information than ever before. In our field, this information was not as significant of a job threat as our complex decision-making, or “decision-making asymmetry,” insulated us from the flattening of the internet. This later, subtle gap in decision-making is now being bridged at warp speed by sophisticated neural networks. As a result, we will have to become data scientists as much as we are clinicians. Instead of avoiding this technology, we must run toward it and understand machine learning at a visceral level. We should be instrumental in guiding the design and deployment of sophisticated models that involve a constantly expanding decision matrix while continuously ingesting more data in order to outperform its prior version. Medical school curricula should ditch memory-based regurgitation and focus more on producing physicians that are capable of the highest level of analytics.
We need to learn and be trained on how to integrate machine learning into every component of our practice and design, even if it means offloading previously extolled elements of patient care. Realistically, this shift in mindset will benefit patients the most. While we clearly have the edge at this moment in time, I worry the route of innovation is indifferent to our obsolescence and will continue to remain indifferent. When I was in medical school, I heard of warning signs that “all of us would be working for the (nefarious) mega-hospitals.” Now, I worry we will be out of work altogether unless we redefine our basic value proposition.
If my sprinkler system will automatically shut down the sprinklers when rain is imminent, what is keeping sophisticated neural networks from “automatically” processing my age, demographics, and every single lab result ever drawn on me since birth to pre-treat any disease before it could even be diagnosed? And in that world, how do we stay relevant?
Where do you see machine learning's role in medicine? Share in the comments.
Dr. Chirag Parghi is a board certified radiologist with fellowship (subspecialty) training in Breast Imaging and is the proud Chief Medical Officer of Solis Mammography. His clinical interests are focused on the early detection of breast cancer. Dr. Parghi has been practicing radiology in the greater Houston area for 8 years, and obtained his MBA from University of Houston. He is a 2021–2022 Doximity Op-Med Fellow.
Illustration by April Brust