It’s one thing to make the choice to spend your career fighting to save lives; it’s another thing altogether to come face-to-face with the harsh reality of death. As a third-year medical student, my trauma surgery rotation highlighted that distinction. For all the patients we saved, there were also those who, despite the team’s best efforts, succumbed to their injuries amid trauma activations. The protocol for a patient’s death in the trauma bay was always followed to a tee: The attending would call for dismissal of the activation, the time of death would be stated aloud, and then a moment of silence would commence. The silence would be abruptly broken by the chief resident as she called for me and the three other medical students on the team to meet in the workstation for a debriefing session. “Does anyone have any reactions to what we just saw?” she would ask. Each traumatic death was rife with its own shocking imagery. I had felt the skin of a pulseless human being become cold. I had seen limbs in paper bags labeled “left” and “right.” I had stood one foot away from a resident forearm-deep in the chest of a hemorrhaging patient. I had heard family members identify their loved one. And with each death, I would sit in a makeshift circle of chairs surrounded by my peers and the chief resident in the middle of the trauma workstation. Surely, I should have had a reaction. But, each time, I would sit there blankly and dumbfounded, paralyzed by the thought that I saw everything and felt nothing in real time.
I refrained from reflecting much at the hospital, believing my identity as a stoic and reserved woman of science was sufficient to carry me through to my next day on the job; cue the Arrested Development narrator: “It wasn’t.” Each day, I returned home to the quiet of my apartment, replaying every decision made in the trauma bay. The principle of beneficence is a doctor’s North star; in cases requiring exceptional life-saving measures, however, there are many cases when well-intentioned actions can become harmful. In the absence of a directive from a patient, it’s not always clear whether pursuing aggressive resuscitation of a patient or allowing that patient to pass peacefully would be a more compassionate choice. Coming to terms with the weight of helping make those decisions was overwhelming.
Toward the end of the rotation, I finally shared my feelings with my fellow medical students on the team. Even though none of us had shared our concerns at our scheduled post-trauma debriefings with the chief, I was relieved to hear they were also struggling to process the gravity of what we had witnessed. Together, we relayed our concerns to the attending physician. He explained that because deaths in the trauma bay may be abrupt and chaotic, it’s often challenging to reflect on our own responses shortly after the adrenaline-fueled urgency of the moment. He then tearfully shared a memory during his trauma training when his team did not pursue intubating a patient, as the family understood intubation would not change their loved one’s fate. The patient passed away within minutes surrounded by family. His story had a calming effect on me; hearing a seasoned trauma surgeon share an emotional moment from his career felt like being granted permission to feel the emotions that a person should feel when they hold human lives in their hands.
Of course, it’s often necessary for clinicians to compartmentalize so they can effectively treat patients during a crisis. But I refuse to accept that we need to become “desensitized” to our most intense moments on the job. Each patient we treat — those we save, and those we fail to save — can and should leave a mark on us. It’s been a process learning to give myself time to reflect and feel the emotions at the right time, especially because it doesn’t feel like these conversations should be a priority when there is always another patient to treat. Now that I’ve talked with my colleagues, I’m grateful to those who have helped me cope with the emotions that come with the high stakes of trauma surgery, and I’m proud to work alongside other medical students, residents, and attending physicians who can be professional without losing sight of their humanity.
Ariel Brown is a fourth-year medical student at UT Southwestern in Dallas, TX.
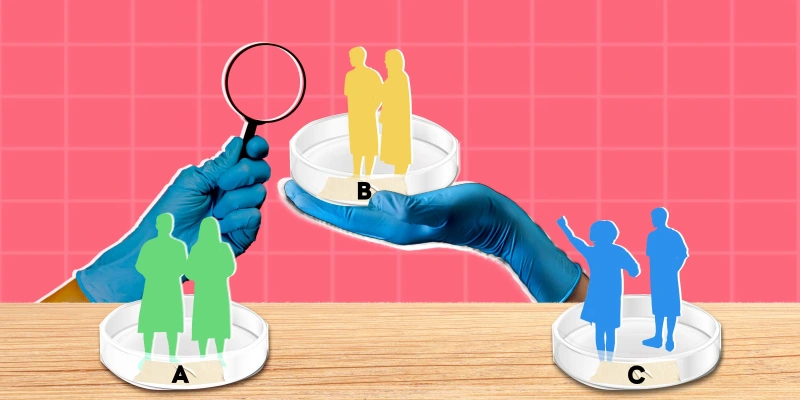
Illustration by April Brust