Time of death for my first patient of the day: 10:25 a.m. Three hours later, the room was cleaned and filled with a new patient. The chemical smell of bleach had barely faded and the memories of the prior patient were still fresh in my mind — but I had no time to linger on the thoughts when there was another patient who needed my immediate attention. Little did I know that by the end of this shift I would have pronounced three patients dead. This was the new reality for me and my colleagues while working in the COVID-19 ICU.
By the end of summer of 2020, I had had enough. Working overtime in the ICU, with countless patient deaths and no end in sight, the stress was becoming unendurable. Toxic thoughts flooded my mind and the term “burnout” became all too prevalent in my day-to-day dialogue.
At the time, I was a novice nurse practitioner wondering how this had become the start to my long-awaited career as a critical care NP. I had not yet built my skill set of stress management, although it may not have mattered with the weight of the pandemic pushing everyone down. With little experience on how to manage the challenging environment, I felt lost and anxious. Burnout was already staring me in the face, and I realized there was no other option than to develop a routine and create tools to pull myself through.
The ICU is highly stressful and intense even when not in the midst of a pandemic, and critical care clinicians deal with rare and unique problems on a daily basis. Even the most mentally tough and emotionally intelligent clinicians know that they will be challenged — and that as a reward, they will save many lives and help to ease the suffering of those they cannot. This responsibility, while highly fulfilling, can catch us off guard if we do not treat ourselves with the same compassion and patience as the people under our care.
During my search to find techniques to manage my stress level, I noted several different things that worked well. Aside from the usual healthy diet, exercise, and adequate sleep, there were other practices I used that could benefit other ICU clinicians or anyone that struggles with similar hardships.
First, I began to journal about my patient experiences. This was a way for me to rewrite the feelings and memories of what I had been through so I could reflect on my emotions, acknowledge them, and move forward. As I wrote, I was able to glean lessons from the thoughts and feelings and learn how to approach a situation differently in the next patient encounter.
One topic I felt I struggled with in the beginning of my career was discussing end-of-life with patients, including their goals for their last moments. I wrote about this in my journal often to keep it front of mind. Doing so helped me push through the discomfort and strangeness of the end-of-life process.
Recently, I had a particularly profound end-of-life conversation with a patient. He had advanced heart failure with no options for transplant or a mechanical device to keep his heart pumping, and many decisions were being made about him but not with him. I went into his room one morning, sat in the chair next to him, and talked with him for half an hour about life, what he would want his next few weeks or months to look like, and how family was so important to him. We ended on a constructive note and decided to have his family come to the hospital and discuss hospice so he could be at home with them. Had I not reflected often on how to handle these situations through my journaling, I may not have helped this man have such a positive end-of-life experience.
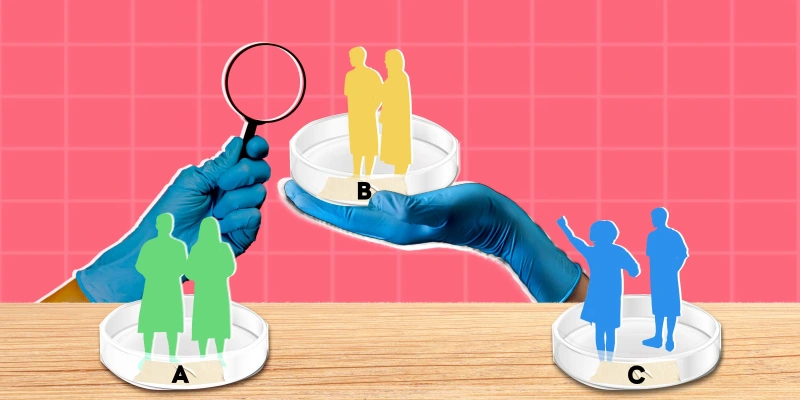
Second, I began to discuss my patient experiences and the emotions I was experiencing with other colleagues. What I came to find was that I was not alone. Going through hardships is one thing, but finding people with the same experiences is powerful. Opening up allowed me to meet people I could be candid with about our shared struggles. I would listen to how they handled certain situations and what they would have done differently. Talking through these situations gave me comfort and the knowledge that if I struggled in the future I would have a support system to turn to — a tribe.
Third, I reached out to a therapist. I had never sought out therapy prior to this point in life, but the stress I was facing in the ICU was unprecedented. After therapy, to say the change I saw in my attitude was profound would be an understatement. My therapist gave me tools I would have never come up with on my own and unlocked thoughts and emotions I needed to walk through. One simple trick she taught me was to pause in a moment of perceived stress and go through my five senses. I would sit for a brief minute, take a deep breath, and note what I could smell, taste, hear, feel, and see. This simple grounding technique would help me pause and prepare for a difficult discussion or allow brief interruption in a hectic moment so I could move forward.
My question now is, how can we as health care professionals ensure we are taking care of ourselves adequately in order to take care of our patients? I believe starting with some of the above tools, and using them consistently, is key. Change I hope to see or be a part of advocating for would be to create in-hospital support groups for health care clinicians to discuss their stressful experiences and promote more hospitals and employers to offer free counseling to clinicians and other health care staff. In a society where suicide and burnout are so prevalent, these changes shouldn’t simply be considered, they should be implemented with vigor. We don’t have to be burnt out or stressed beyond our limits, but we do have to support each other.
What are your strategies for mitigating stress in intense environments? Share in the comments!
Kymberley Filip is an ICU nurse practitioner in Houston, TX at Baylor College of Medicine. She has been taking care of critically ill patients for over seven years. Born and raised in Texas, she attended The University of Texas at Austin and is an avid Longhorn fan. Kymberley is a 2023-2024 Doximity Op-Med Fellow.
Image by ina9 / Shutterstock