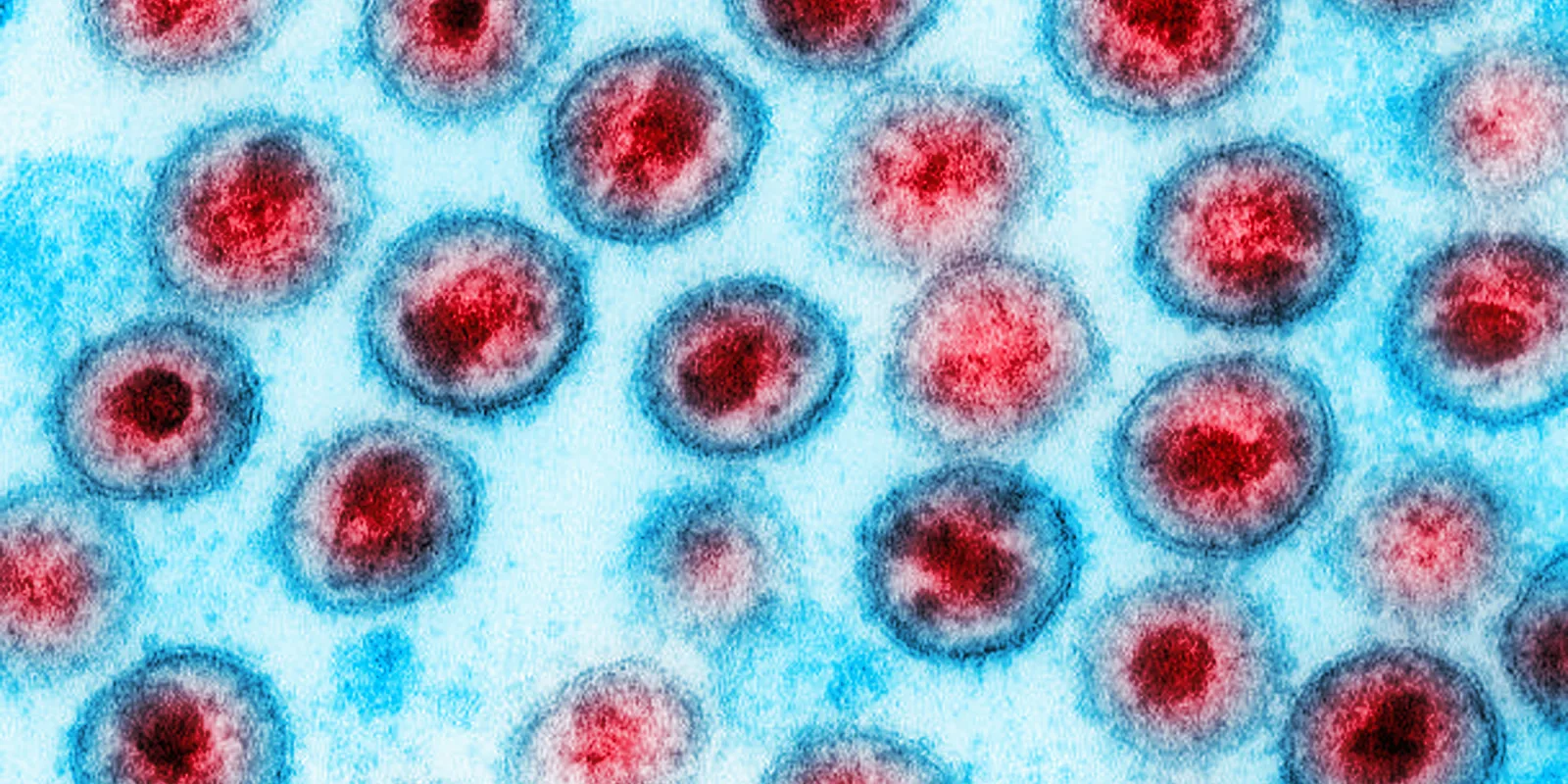
Countries in sub-Saharan Africa, the region with the highest burn of the human immunodeficiency virus (HIV), have incorporated the use of pre-exposure prophylaxis (PrEP) into national HIV-prevention strategies. It is estimated that more than one-third of people receiving PrEP worldwide are in Africa. During IAS 2021, Parikh et al. presented data on Antiretroviral Therapy Resistance (ART) in persons diagnosed with HIV after PrEP rollout in sub-Saharan Africa.
Monitoring for HIV resistance among patients receiving oral tenofovir disoproxil (TDF)-based PrEP is essential. PrEP breakthrough infections could result in acquiring resistance mutations that may lead to virologic failure. Additionally, transmitted resistance from failing antiretroviral therapy could lead to PrEP breakthrough infections. In general, ART resistance among patients getting PrEP is rare and most commonly detected in patients with undiagnosed HIV infection at the time of PrEP initiation. Among patients who acquire drug resistance while on PrEP, M184V and K65R are the most commonly identified mutations.
Global Evaluation of Microbicide Sensitivity (GEMS) Project Team monitors HIV drug resistance in PrEP rollout programs in sub-Saharan Africa with more than 104,000 persons on PrEP. In this observational study, blood samples were collected from participants diagnosed with HIV while on PrEP. Samples were tested for HIV drug resistance mutation and TDF levels to evaluate medication compliance. Of the 104,000 participants on PrEP, 229 had seroconverted over four years. Most seroconversions happened in the first 6-months of starting PrEP (55%), while seroconversions after being on PrEP for more than a year were uncommon (18%).
When evaluating for the presence of resistance mutations, 55% of participants who seroconverted had no acquired resistance while 23% had acquired resistance mutations associated with PrEP, and 22% had background transmitted resistance that was unrelated to PrEP. M184I/V was by far the most common acquired mutation, while K65R mutations were noted in four participants. Additionally, various Non-Nucleoside Reverse Transcriptase Inhibitor (NNRTI) mutations were noted. Among participants with PrEP associated mutations, high TDF levels were noted, indicating high rates of adherence.
This study demonstrates how effective PrEP is in preventing HIV with incidence of new infections around 0.2%. However, among patients who are on PrEP and experience HIV breakthrough infection, there is a high risk for acquiring resistance mutations. Both background transmitted resistance and PrEP associated mutations are noted. Accordingly, frequent HIV testing and monitoring for development of HIV drug resistance while on PrEP is essential to preserve future ART options.