Less than a year into a new job as medical director at a health insurance company, it surfaced that I had retained a small percentage of ownership in my former group practice. I never disclosed it to the company, and quite frankly, I didn’t think it was necessary. However, in order to remain employed, I was required to sell my stake in the practice. The CEO informed me that he was being “kind” by letting me stay with the organization, and that undeclared conflicts of interest such as mine were grounds for immediate termination, as I might preferentially steer patients to that practice over others, and I stood to profit from that arrangement.
I divested my portion of the practice, but due to my initial lack of compliance (failure to report the conflict), I was quietly fired – allowed to stay with the company but demoted in position and moved to a basement office in a satellite location. Essentially, I was managed out, and I left the organization not long afterward.
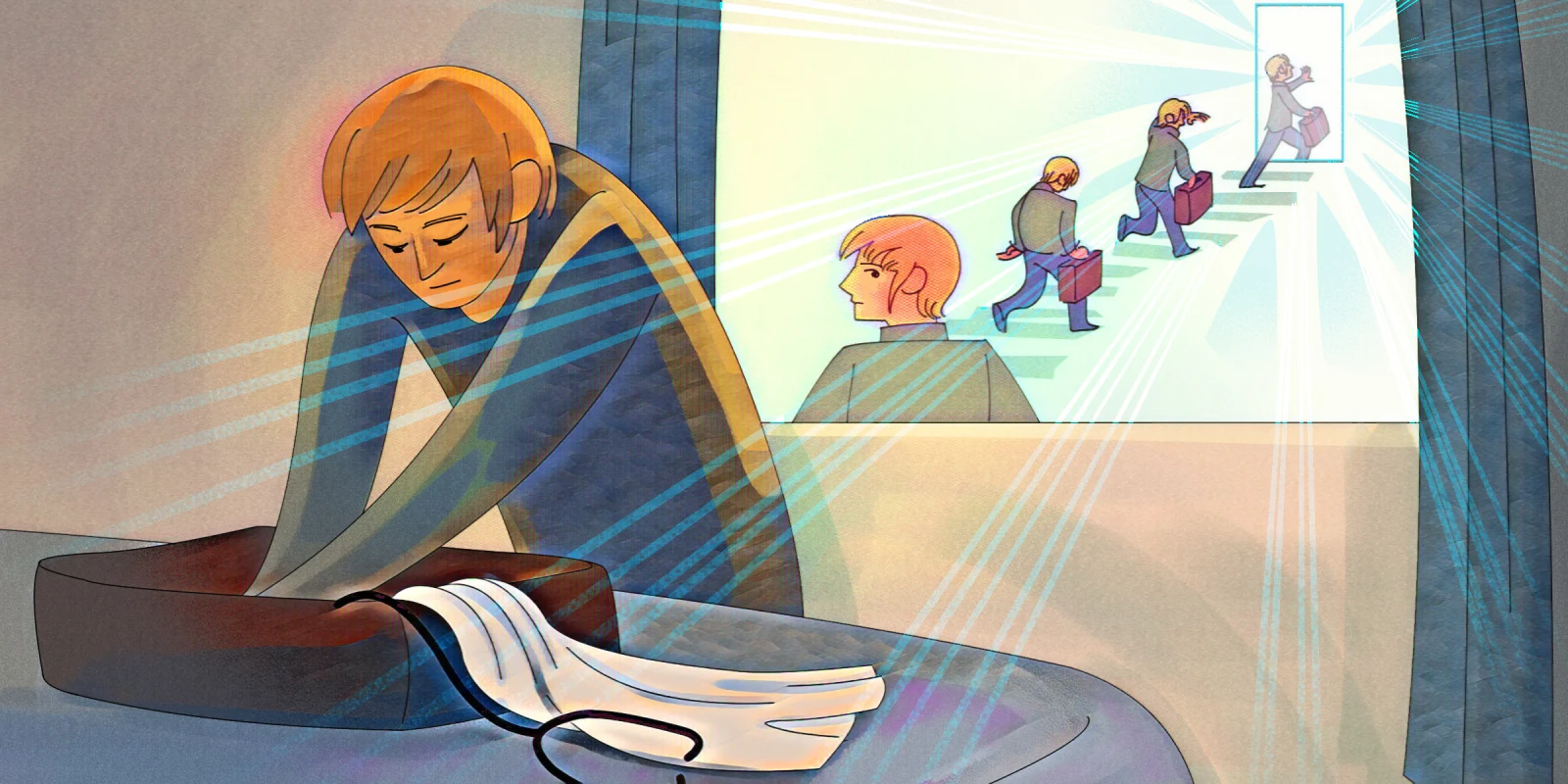
What Is Quiet Firing?
“Quiet firing” refers to a situation where an employer subtly pushes an employee to resign rather than directly terminating their employment. This can be achieved through various means, such as gradually stripping away significant duties and responsibilities, excluding the employee from important meetings, projects, or decision-making processes, providing consistently negative feedback without basis or constructive criticism, denying promotions, raises, or professional development opportunities, assigning tasks that are excessively difficult or impossible to complete within given deadlines, and creating a work environment that is uncomfortable or hostile, making the employee feel unwelcome.
Physicians might be quietly fired due to failure to meet evolving productivity targets, disagreements with administrative decisions, or persistent clashes with colleagues or superiors. Furthermore, changes in hospital policies, restructuring, or a shift toward more profitable specialties can result in decreased support, undesirable shifts, or reduced responsibilities, making the work environment untenable for the physician. This approach allows institutions to avoid potential legal disputes and public backlash while gradually encouraging the physician to leave voluntarily.
A quiet firing can have significant professional and personal implications. Physicians may find it challenging to secure new positions if they leave their current role under such circumstances. Negative performance reviews and lack of recent achievements can impact their professional reputation. A physician experiencing quiet firing might be distracted or demoralized, which could negatively affect their ability to provide high-quality patient care.
The stress and uncertainty associated with quiet firing can lead to burnout, anxiety, and other mental health issues. Additionally, physicians need to ensure they are complying with medical and ethical standards despite the difficult work environment. Quiet firing tactics could indirectly pressure them to compromise on these standards. Being quietly fired can strain relationships with colleagues and patients, which are crucial for successful medical practice.
One physician described his quiet firing this way: “…often subtle but firm pressure, manipulative changes, and general discomfort designed to make you want to leave. It is a cold, calculating, passive-aggressive business approach to help guide a person away from continued employment. At first, you may think it is a small event that you simply overlooked, but those events quickly add up and escalate. Your work is never good enough, your approach is overlooked, you might even be ignored, and over time you wonder how you could even improve. Could this truly be your problem, or is something else at play here? Eventually, time, examples, and intuition tell you something is not right.”
What You Should Do If You Are Being Quietly Fired
Physicians who feel they are being quietly fired can take several steps to address the situation. They should keep detailed records of changes in responsibilities, performance reviews, and any communication that might indicate quiet firing. Attempting to have open and honest conversations with supervisors or HR about their concerns and seeking feedback is important. Engaging with professional organizations, mentors, or legal counsel can help them understand their rights and options.
I never sought legal advice on the matter, but my research has led me to believe that there is no definitive answer to whether a physician employed by a health insurance company can retain partial ownership of an in-network group practice. I imagine I should have consulted a legal expert before starting the job to ensure I was in full compliance with all relevant laws and company policies. Better yet, I should have declared the conflict upfront whether or not I believed it was relevant. This is what virtually all corporate compliance officers will advise new or potential hires, and it would be prudent to seek out legal advice of your own if you suspect quiet firing.
If you try to hang in there as you are being quietly fired, be prepared to be treated poorly while seeking affirmation and answers from colleagues. You must prioritize your mental and physical health, take a step back, and view the situation objectively. Would you advise a family member to keep enduring, taking punishment, and asking for more? Understanding the dynamics of quiet firing and its implications can help you navigate the situation more effectively by knowing when to leave and protecting your career and well-being.
I knew it was time to leave within a few short months as my responsibilities gradually shifted and became mundane. My role was diminished and no longer aligned with my skills and interests. The isolation excluded me from important meetings and decisions. My efforts were being deliberately overlooked. I realized my professional development would be limited and there would be no opportunity for career advancement.
I looked for new employment, and I timed my exit with a new job, protecting my career by telling my new employer that my old job was no longer a good fit. I was careful about my language regarding my former company on the way out. I wasn’t worried about a relatively short stint appearing on my CV and what that might signal. The average medical director stays at their job for a few years, and physicians in full-time corporate practice also seem to change jobs quickly. In my experience – and I believe HR personnel would attest to this – the gold watch is a relic of the past.
What is your experience or knowledge of quiet firing? Share in the comments.
Arthur Lazarus, MD, MBA is a former Doximity Fellow, a member of the Physician Leadership Journal editorial board, and an adjunct professor of psychiatry in the Lewis Katz School of Medicine at Temple University in Philadelphia, Pennsylvania. He is the author of several books on narrative medicine, including Every Story Counts: Exploring Contemporary Practice Through Narrative Medicine, and Narrative Medicine: Harnessing the Power of Storytelling through Essays.
Illustration by April Brust