“You. Yeah, you,” said Dr. Stewart with a stern voice and pointed gaze in my direction.
“So what do we got here in Room 3?”
The sun had barely risen and started to beam through the floor-to-ceiling windows of the medical ICU on the seventh floor of the inpatient tower. I was a third-year medical student and was up all night assisting my senior resident in the care of my critically ill patient. Despite the beeps and alarms of ventilators, IV pumps, and patient monitors, I could hear my heart pounding in my chest as I was about to present to Dr. Stewart, my attending physician.
After fumbling through my notes in the large inner pocket of my short white coat, I went for it. I described how the patient was admitted by the ER for shortness of breath, was found to have severe pneumonia, and how his clinical course acutely worsened overnight, resulting in his current state of being on a mechanical ventilator with a central line in place, infusing broad spectrum antibiotics and vasopressors.
I handed Dr. Stewart the clinical progress note that I had written (yes, hand written) just before rounds, feeling cautiously optimistic.
He scanned through it quickly until his eyes fixated on the bottom of the page, where my “assessment and plan” section said “shortness of breath” as the principal clinical problem.
“This is an excellent progress note,” he said. I was ecstatic internally, but I totally kept my cool.
“Thank you, sir,” I calmly replied.
“Excellent for an urgent care down the street if this guy popped in on his lunch break with a snotty nose,” he retorted. Before I could say anything further, it was on to the next patient.
I was baffled.
Later that morning, Dr. Stewart was at the nurses’ station with a stack of patient charts in large three-ring binders doing his clinical documentation. I couldn’t shake the feeling of having completely blown it earlier during rounds, so I gathered the courage to approach him and ask him what he meant by his “urgent care” comment.
He then pulled out my progress note from the patient chart, and in his attending attestation portion had written “septic shock complicated by acute hypoxic respiratory failure” as the principle problem. He then pulled out what appeared to be a scroll of hieroglyphics that said “Super Bill” across the top and had several columns of numbers that had the letters “ICD” next to them.
“Your clinical assessment was fine. But, we’re in the ICU treating a critically ill patient, so we have to document that accordingly to make sure the progress note reflects the highest complexity of care management. Billers and coders look at everything. So, you’re going to have to learn to speak their language.”
Clearly, I had no idea what he was talking about.
“Don’t worry,” he said with a wry chuckle. “I’m sure you’ll get it eventually.”
Out of all the medical knowledge and life experiences I gained throughout my medical training, this experience with Dr. Stewart was the most valuable. This was one of the key moments that I realized that despite being blessed with education and training from top tier universities in the U.S., I was actually undertrained — severely undertrained at that — at basic concepts regarding business in medicine, such as how doctors actually earn money.
I went through my medical school curriculum and asked several residents when in our training we learn the concept of billing, coding, and you know, insurance stuff.
The consensus was clear: We don’t.
My experience with Dr. Stewart also resonated with me in a very personal way. At that time, my father was nearing his 30th year of private practice as a gastroenterologist, with my mom at the helm of managing the practice. Throughout my childhood and into my adult life, I had a front row seat to how much time, energy, and effort it takes for a physician to simply get paid for services rendered. Some of my most memorable moments of being a kid were my parents taking me to basketball practice and then coming home to help my mom stuff envelopes after I finished my homework. I watched them masterfully navigate the increasingly complex health care system all while raising a family.
But this put me at a crossroads that day in the ICU. I didn’t have 30 years, I thought. I didn’t have a private practice to learn from. I may get it eventually, but what about now?
That brought me to ask myself a central existential question:
Why do medical students and trainees not receive any formal training in medical billing, coding, insurance practices, reimbursements, and what work RVUs are? With all the money that doctors spend on education, why are we not taught how to actually make some of it back?
Based on this experience and a number of others that were similarly enlightening, I decided to take time away from medical school before residency and pursue an MBA degree. Being a science major as an undergraduate, I never really had the time or opportunity to devote significant effort to studying disciplines like economics, finance, accounting, and operations.
This was one of the best life decisions I have ever made. During business school, I made it a point to educate myself as much as I could on matters of health care economics, finance, operations, and revenue cycle management. Being surrounded by business professionals as classmates who were experts in their own fields was an incredibly vulnerable feeling but incredibly rewarding at the same time.
As I transitioned back into clinical training, I was then able to apply what I had learned in business school through quality and process improvement projects in the hospital successfully to the benefit of others. I also gained valuable experience learning how to work with hospital administration even while still in residency.
About six months into my first job as a gastroenterologist out of fellowship, I wanted some insight into my wRVU productivity, so I went to the chief financial officer of my hospital and asked for six months’ worth of my productivity data.
I was shocked. My clinical productivity was in the 45th percentile according to national Medical Group Management Association data.
So I called my mom. “Mom,” I said. “Something’s not right. I’m working my tail off but I’m only at 45th percentile.” “Don’t worry,” she replied. “We’ll figure this out.”
For the next four months of my professional life, my second full-time job was personally auditing the raw data and charges submitted for every clinic visit, every inpatient consultation, and every endoscopy procedure I performed, and analyzing it together with the help of my parents. Eventually, I was able to discover that the appropriate modifiers on my endoscopy procedures were not being captured correctly, resulting in approximately 500 wRVUs of under-billing.
When I finally received my revised productivity report (and paycheck), I found myself feeling exactly the same as I did sitting next to Dr. Stewart in the ICU — baffled.
Essentially, I needed a formal business degree, years of experience in working with hospital administration, masterful capabilities in Microsoft Excel, an extra approximately 20 hours per week, and my mother JUST to collect dollars that I rightfully earned by providing quality patient care.
I shared this experience with one of my ENT colleagues in the hospital cafeteria one day, and without looking up from his salad, he casually said, “Yeah I just submit everything as a Level 3. I don’t have the time or brains for any of that.”
And then it really hit me. How many other physicians at my own hospital, or in my home state, or nationwide for that matter, are getting ripped off because they either don’t know the right questions to ask or simply don’t have the time?
I have since transitioned back into academic medicine and I am now a GI attending physician at a major academic university. In my role as a clinical educator, I have made it my personal mission to teach medical students, residents, and fellows, as much as I possibly can about coding, billing, and how to be prepared to actually be a doctor, apart from the clinical part.
But at the end of the day, I am just one man on a mission based on my own story. There is so much work that needs to be done in order to provide a more well-rounded education for our future physicians. As much as I am grateful for all the positive feedback I receive from my trainees, I am equally disheartened at the sideways looks and disapproving comments I receive from colleagues about “tainting” the trainees education with such a seemingly taboo subject such as reimbursement.
In order for our future physicians to succeed in practice and not succumb to the corporate practice of medicine, these barriers must be broken. Physicians are intelligent, resourceful, courageous people. We practice these traits every day at the bedside, so why can’t we apply these values to provide for our families?
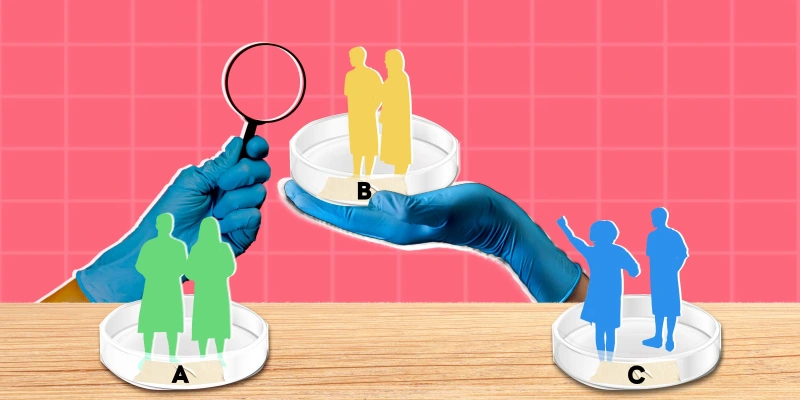
Currently, the ACGME has a general category for competency in “systems based practice” for medical trainees, but there are no formal curricula or guidelines on how to hardwire teaching the business of medicine in medical schools and training programs across the country. As leaders and educators in medicine, we need to start prioritizing giving our next generation of physicians the tools they need to succeed as business professionals in the health care industry.
Hopefully, by joining me in this effort, Dr. Stewart would be proud. And hopefully my mom and dad would be too.
How do you make sure you're reimbursed properly? Share in the comments.
Dr. Neal Kaushal is a gastroenterologist in Oklahoma City, OK. He serves as executive director of general GI and endoscopy at OU Health (hospital of the University of Oklahoma Health Sciences Center). He also has a specialty in business operations and is passionate about the intersection of business and medicine to support patient access to care. He enjoys playing ball and going on walks with his three Dobermans, Rani, Riya, and Rishi. Dr. Kaushal is a 2024–2025 Doximity Op-Med Fellow.
Animation by Jennifer Bogartz