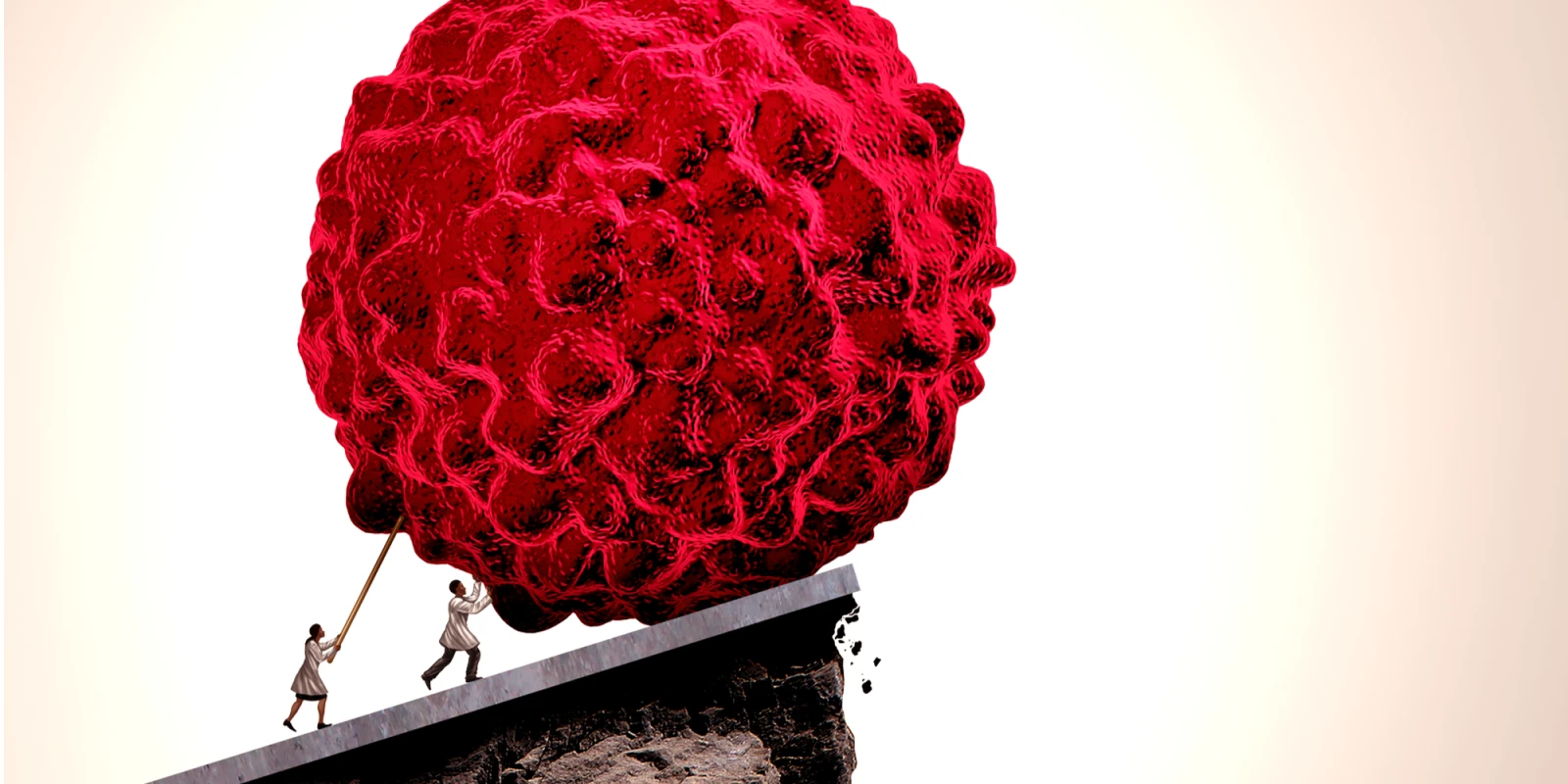
Author's note: people with stage IV lung cancer are becoming long-term survivors. Not just in clinical trials. They exist in my rural community oncology practice. In this post I share how the era of immunotherapy, specifically immune-checkpoint-inhibitors, has changed the landscape of practice in metastatic non-small-cell lung cancer (NSCLC) for clinical community oncologists.
I want to start by telling you about Joe (name and some details changed to protect anonymity).
In 2015, Joe was diagnosed with stage IV NSCLC adenocarcinoma. He had a massive metastasis to the liver, taking up at least half of the organ. He also had two small brain metastases causing vasogenic edema. I consulted on him in the hospital. I laid out the diagnosis and how the cancer was affecting his body. He was in his early eighties and seemed frail. He had a stroke a decade ago that left him with residual deficits. He had severe osteoarthritis that limited his mobility. I described the options for treatment from full treatment (palliative) to supportive care and hospice. I told him, in frank terms, of the limited prognosis. If I’m honest, I tried to steer him toward hospice and was somewhat surprised when he opted to try for full treatment. He had stereotactic radiosurgery (SRS) to treat the two brain lesions, and after, I started him on single-agent chemotherapy as it was my clinical judgment that his performance status was not adequate for a combination regimen. He had a good response in the brain to the SRS, but no response in the liver to chemotherapy.
This was summer of 2015. In May of 2015, the first immune-checkpoint inhibitor had been approved by the FDA for NSCLC in the second-line metastatic setting. I had started two other of my patients on it by that point, and both were tolerating it well. I discussed the option with Joe, and he wanted to proceed.
At three months, the primary lung tumor and the liver metastases had decreased in size. By nine months, the largest liver metastasis had shrunk by 80%.
At ten months, he presented to the Emergency Room with an immune-mediated toxicity. He responded to prednisone, but we had to stop the immune-checkpoint inhibitor. I planned to keep him off treatment, follow serial imaging, and consider a cautious restart of immune-checkpoint inhibitor at the time of disease progression, which I counseled him to expect within six months. That was over two years ago.
I see him back with imaging every three months. He has yet to progress. He remains off any treatment.
I want to re-state it so that it can sink in. My patient is in apparent remission from stage IV NSCLC, after nine months of immune-checkpoint inhibitor, and remains off therapy for over two years.
I have a cohort of long-term NSCLC survivors in my practice now. Both those who started in second-line or beyond, and more recently, those who started it as first-line therapy. The responders all continue on immune-checkpoint inhibitors because we don’t know when we can stop them, and for whom we can stop them, and at what point. For Joe, we were forced to stop for toxicity. In the others, without toxicity, we continue the treatment on an open-ended basis. The first two patients I mentioned above, who I started on treatments in the summer of 2015, the same year as Joe, also continue on them. That means they’ve been living with stage IV NSCLC for over three years.
After two years, I sent one of the patients for aortic artery aneurysm (AAA) repair because I could no longer be certain that the lung cancer would kill him before the AAA would. He had the AAA repair and did great.
NSCLC is but one example of how immunotherapy has upended the paradigm of expected limited survival in advanced cancer. In my cohort of long-term NSCLC survivors, I have to pay attention to their comorbidities. To no surprise, they have other tobacco-related comorbidities, especially coronary artery disease and peripheral vascular disease. Some of them, to my eternal frustration, continue to smoke tobacco. Like my patient with the AAA repair, I have to convince my colleagues that we need to treat and manage their other medical conditions as we would in any other patient. We can no longer push their comorbidities to the back burner because the patients are not expected to live past six months.
This is an awesome problem to have. Oncologists can, in some settings, now tell our NSCLC patients they are less likely to die of their cancer than something else. But we still need to treat the “something else.” And we cannot do it alone. As our practices fill with these long-term survivors, the shortage in medical oncologists grows, and the gap between the care needed and the care we can provide widens to an insurmountable magnitude.
Although the societal stigma surrounding cancer has become less and less over the past several decades, I still bump up against it in the medical world. “Why bother?” was the attitude of some on the inpatient team when Joe opted to try full treatment in 2015. Joe himself is the best answer to that question I could ever give.
Image by Lightspring / Shutterstock
Dr. Jennifer Lycette is a community oncologist, mom, and writer. She blogs at The Hopeful Cancer Doc, started in 2017 with the idea to promote hope for physicians, both in practice and life outside of work. She writes about the intersection of doctoring and life, and the challenges physicians face in this unprecedented healthcare era. Some of her narrative essays have been published in medical journals including NEJM and JAMA. She lives and works in Astoria, OR with her husband and three children, where she practices and advocates for rural oncology quality care. She is also a 2018–2019 Doximity Author.