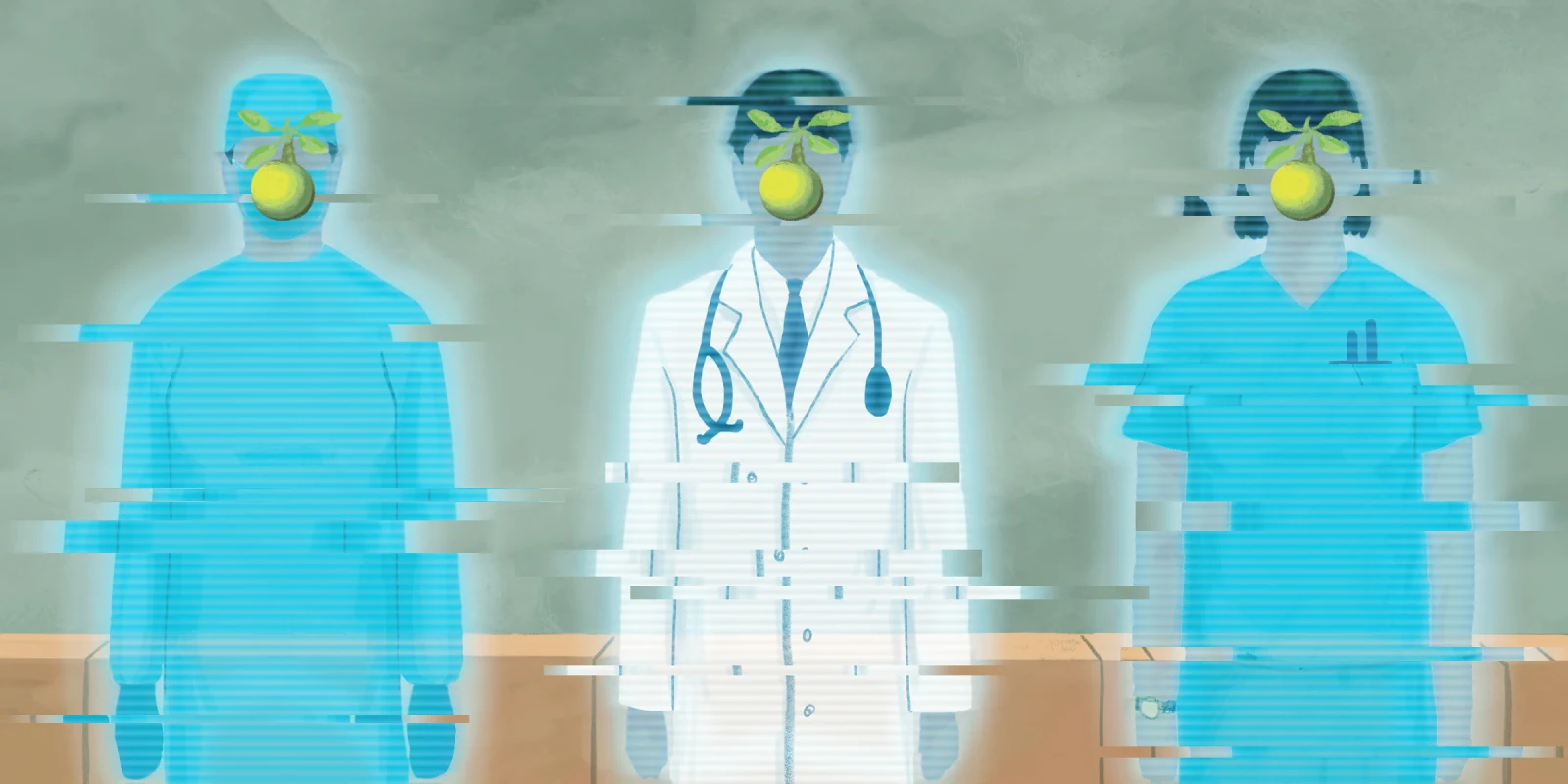
The unprecedented advancement of computer science represents a significant milestone of our time. Recent developments enable the application of algorithms and artificial intelligence in numerous fields, including medicine, which have a significant potential to enhance patient outcomes. For instance, sophisticated decision-making and diagnostic algorithms can address potential knowledge gaps in human physicians or ensure that all potential diagnostic avenues are explored.
Despite this seemingly overwhelming analytical capacity, human doctors still have one unassailable advantage over machine medicine: the ability to improvise.
Computer programs are great at responding to known situations and making objective recommendations based on learned information from available data. But real life is always one step ahead of expected circumstances, and today’s AI cannot be trusted to improvise when lives are at stake and facing new circumstances.
During my volunteer work in Haiti after the 2010 earthquake, which leveled much of Port-au-Prince, I recognized the value of medical improvisation.
My colleagues and I flew in a borrowed private plane stuffed to the gills with medical supplies. The restrooms were stacked floor-to-ceiling with supplies, and the aisles were so tightly packed that the doors could not be opened.
Upon arrival in Port-au-Prince, a hospital was nearby — but we couldn’t use it. The enormous building was considered so dangerously unstable that it might collapse at any time, crushing anyone unfortunate enough to be inside it. Instead, we were given the green light to use a small private surgical clinic in a single-story building.
This building had an OR but no electricity. Our lights were powered by a tiny generator that was incompatible with the facility’s equipment sterilizers. In the eerie shadows beyond the lit field, we could see black cracks in the walls where the earthquake had damaged them.
Yet we needed to operate. Hundreds of residents were suffering from crush injuries — injuries that would kill them unless we could amputate their damaged limbs.
So, we operated. Worse, we had to amputate with no electricity and no adequate sterilization procedures. Hand saws were brought out. I think it was one of the surgeons who thought to fill a bucket with betadine and thoroughly dip and swish every piece of equipment that was going to touch a patient. With hundreds of patients lined up outside, at risk of death without a speedy amputation, we had no better options.
Similarly, I have seen many other examples of human improvisation resulting in unforeseen triumphs during 21st century medical disasters. For instance, during the Ebola outbreak in 2014–2016, one African woman developed a technique for creating surprisingly effective PPE by carefully layering duct tape and garbage bags when medical-grade PPE was unavailable.
During the COVID-19 pandemic, we witnessed local knitters improvise unique loops to hold the straps of N95 and surgical masks so that they didn’t pinch the ears of health care workers, who were now forced to wear them 16 hours a day. They delivered these to hospitals.
These examples raise the question of whether AI algorithms could have generated these novel alternatives in the face of unexpected challenges and conditions.
This shows ample room for improvisation in medicine, particularly in resource-poor environments or emergencies.
Real-Life Examples
1) On a British Airlines flight, a surgeon used a knife, fork, and coat hanger sterilized in cognac to insert a urinary catheter with a coat hanger stent for a pneumothorax, saving a life.
2) Improvising an endotracheal tube from a suction tube and a baby bottle nipple or creating a nasal speculum from a coat hanger.
3) Using a handheld injection needle to create an intraosseous line above the medial malleolus is now an accepted part of advanced life support curricula.
4) In areas with limited resources, medical professionals have improvised using items like aluminum foil to control IV flow, disposable gloves as tourniquets, and sterilized single-use syringes for injections.
Transformation into Standard Practice
Successful improvisations often become part of standard clinical practice. For example, the improvised infant ventilator made from assorted parts eventually led to the development of the Baby Bird ventilator, now a standard piece of equipment.
Yet while human ingenuity can turn makeshift solutions into lifesaving standards, technology — particularly AI — often falters when forced to navigate the unpredictable without such creative flexibility.
Self-driving cars have recently shown us the dangers of overtrusting technology. Although they are portrayed as safer and more reliable than human drivers, the cars’ AI decision-making algorithms have nonetheless broken traffic laws and killed pedestrians, motorcyclists, and their drivers. One reason for this limitation is that AI systems cannot improvise when faced with atypical or unexpected situations.
Unlike humans, who can adapt their responses based on context and creative thinking, AI algorithms rely on predefined patterns and learned data. When confronted with a scenario that deviates from their training, they may struggle to generate appropriate responses or solutions. Worse, they may suggest wrong answers or alternatives. This inability to think outside the box can hinder their effectiveness in dynamic environments.
The potential for AI to replace or complement physicians has been a topic of much debate. While AI technology is advancing rapidly and can assist in diagnosing diseases, analyzing medical data, and even suggesting treatment options, the role of a physician involves much more than just technical expertise.
Doctors provide empathy, intuition, and a human touch that AI cannot replicate. They must navigate complex conversations with patients, understand nuanced emotional contexts, and make ethical decisions based on various factors.
Thinking and adapting quickly is essential in medicine, especially under pressure or unforeseen circumstances. This underscores the need for continuous training and preparation for handling such situations. While AI can improve outcomes in many situations by making recommendations, memorizing data, and identifying patterns that human doctors may miss, it will be a long time before I feel comfortable eliminating human doctors from medical decision-making entirely.
What role do you see AI having in medicine? Share in the comments.
Dr. Francisco Torres was born in Seville, Spain, and graduated cum laude from the University of Puerto Rico in 1982 with a degree in biology. He then attended the University of Puerto Rico School of Medicine and was awarded his medical degree in 1986. Dr. Torres performed his residency in physical medicine & rehabilitation at the VA Hospital in San Juan, Puerto Rico, before completing a musculoskeletal fellowship at Louisiana State University Medical Center in New Orleans. He went on to serve three years as Clinical Instructor of Medicine and Assistant Professor at LSU before joining Florida Spine Institute in 1993, and is the author of five books.
Illustration by Diana Connolly