It’s no secret that most residents who graduate programs — medical or surgical — do not seek rural practice jobs. There are lots of reasons for that, personal and professional. But without proper exposure to the day-to-day rewards and challenges of community and rural practice during training, how will young surgeons ever make the decision to pursue rural practice?
One of my favorite rotations during residency was a community hospital rotation about 30 minutes outside of the city. It wasn’t rural, but compared to the tertiary level university hospital where we did most of our training, it felt pretty out there. It was an acute care surgery rotation at a suburban 300-bed hospital. As third and fourth-year residents, we were responsible for seeing new consults, making the decision to operate, running it by our attending surgeon, and then heading to the OR with the patient. The autonomy afforded to us with preoperative decision-making alone was enough to make me giddy. But in the OR too, we were treated with collegiality and respect, rather than the infantilization that surgical residents at academic programs often come to know, dread, and sadly, get accustomed to.
What does any of this have to do with attracting and retaining more rural surgeons? Residents are overworked and really just looking for any silver lining to get them through the day, week, or rotation. A rotation like the one above, though it was sadly only two months out of my five-year clinic residency, taught me so much not just about operating, but about learning how to operate and take care of patients as a nearly independent surgeon. Despite the long days on this rotation, I leapt out of bed every morning, excited and eager to learn and work. The camaraderie found at smaller hospitals is also very enticing. Surgical trainees, especially women and minorities, often face discrimination during training. Rotating at hospitals where the culture and environment are a refreshing change from the cutthroat shark tank of academia can be therapeutic for resident morale.
The residency program I trained at serves the WWAMI (Washington, Wyoming, Alaska, Montana, Idaho) region of patients. This was most evident at our beloved Level 1 trauma center where we routinely had flight transfers in with injured patients from the five-state area. However, it was not until recently, after I had graduated, that the option for a rural surgery rotation became available for residents. This is a huge and promising step toward attracting, training, and retaining much-needed rural surgeons in this large area. The medical school already has done much work in attracting students from the five-state region, with a stated goal of increasing the number of rural physicians who go back to their communities. However, in recent years, there has been a shift, with fewer medical students entering primary care. In order to retain specialists in rural/suburban settings after training, a tantamount effort must be made to increase resident exposure to rural practice in those fields too, not just primary care.
Surgical residents often judge how much they like a rotation based on how much autonomy they get, both operatively and non-operatively, in terms of decision-making for patient care and inpatient management. This of course needs to be earned over time, after experience is gained and sequential levels of responsibility are demonstrated. But oftentimes, autonomy does not come, despite the fact that residency is geared toward making us autonomous surgeons. In discussing favorite rotations with co-residents, we found that we really learned how and when to operate during our community rotations, which unfortunately comprised less than 10% of our total time in residency. This again will be different between academic and community-based residency programs. But ultimately, if we want to attract and retain surgeons in more underserved settings, which in our country often means rural locations, we must expose residents to the benefits of training and working in said environments. One large benefit as a trainee is the opportunity to have different, and often more effective, opportunities to learn. University and urban-based rotations are also incredibly important for training – this is where we see and learn about more subspecialized surgical diseases and operations. But at the end of the day, it is called general surgery residency. Should we not focus more, then, on the general needs of the population, including the population that doesn’t live in the metropolitan cities served by our academic surgery institutions?
Many aspiring surgeons are interested in careers in academics but also want to do service and help underserved populations. While global surgery and global health work is one option, rural surgery is also helping underserved people without having to leave the country. When residency programs highlight and advertise their global surgery opportunities, rural domestic training options should also be included. One does not need to travel across the world to contribute to caring for the underserved.
An important point regarding autonomy and learning in rural and underserved environments: There is an important ethical issue around the higher amount of supervision given to trainees in academic hospitals (often with more economically and socially privileged patients), compared to less supervision at more county/community hospitals. It is rooted in health care disparities and different standards of care that historically in this country have been attributed to patients who are minorities and of lower socioeconomic status. This article is not meant to suggest that rural and community hospitals are better given less supervision and thereby more autonomy for trainees. However, the culture at community, non-academic hospitals does afford a different learning environment that can be beneficial, especially for surgical residents who are trying to make a decision between academic and non-academic practice. This line is often the dividing line between those who choose to stay in urban areas and those who look to work in more remote, rural areas.
Ultimately, I think there are many angles to take to address this need for more rural surgeons. But a practical one is to increase the opportunity for elective rotations in rural settings, and make at least one or two mandatory during training. The moments in residency where, as a budding surgeon, you really feel that you are on the precipice of learning how to become an independent surgeon and clinician, are memorable. I had several such moments on my community rotation. Who knows, those moments may just be enough to change the course of a young surgeon’s career.
If you work in rural medicine, how did you come to practice there? Share in the comments.
Dr. Mohini (Mo) Dasari is a general surgeon in Kirkland, WA. She practices and teaches yoga, writes for pleasure, therapy and advocacy, and loves posting her amateur cooking and baking on Instagram @modalala. Her favorite thing to do is spend quality time with her husband, two-year-old daughter, and seven-pound dog. She tweets at @mdmdaware. Dr. Dasari is a 2023–2024 Doximity Op-Med Fellow.
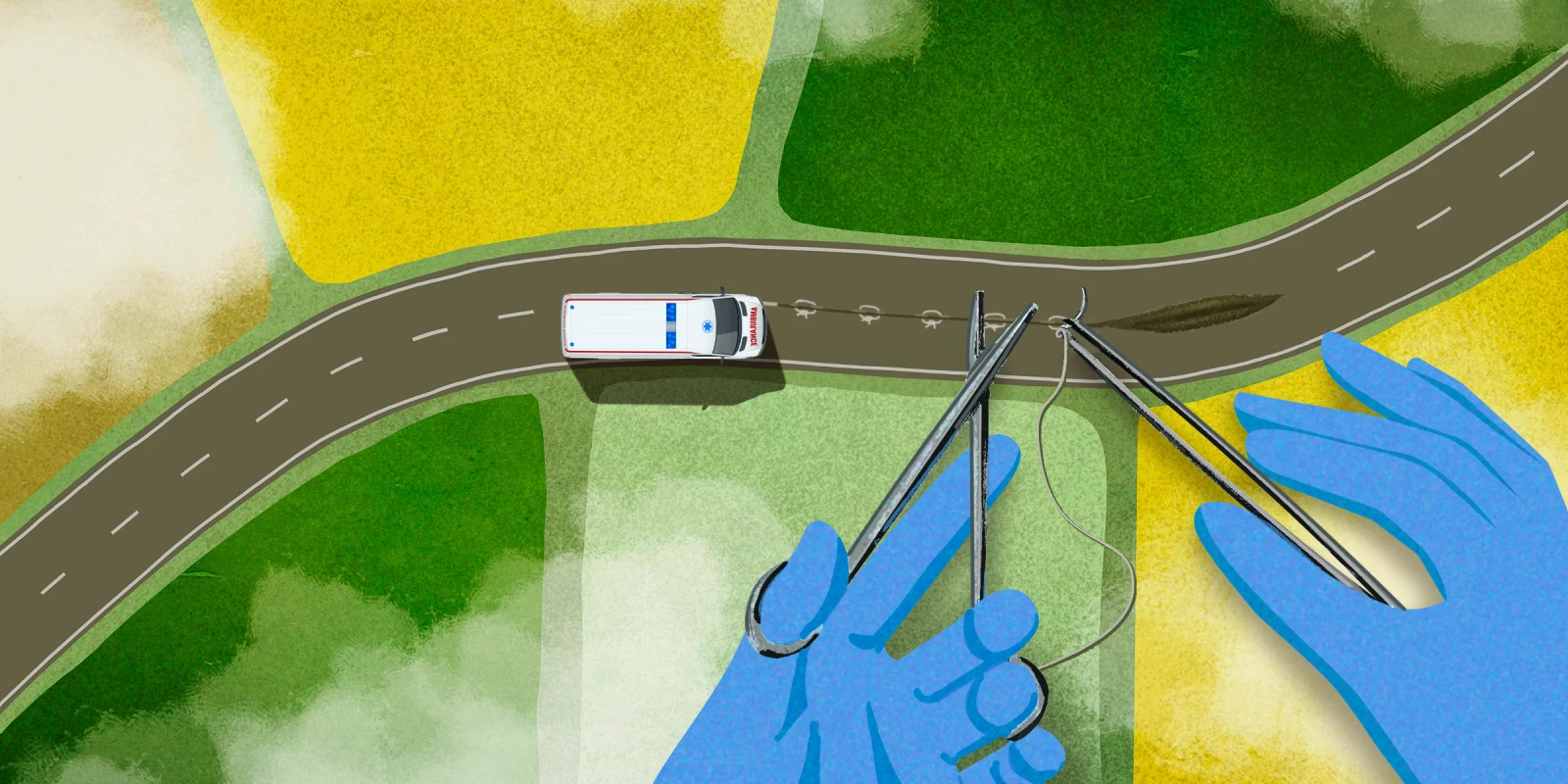
Illustration Collage by Jennifer Bogartz / Getty Images / Shutterstock