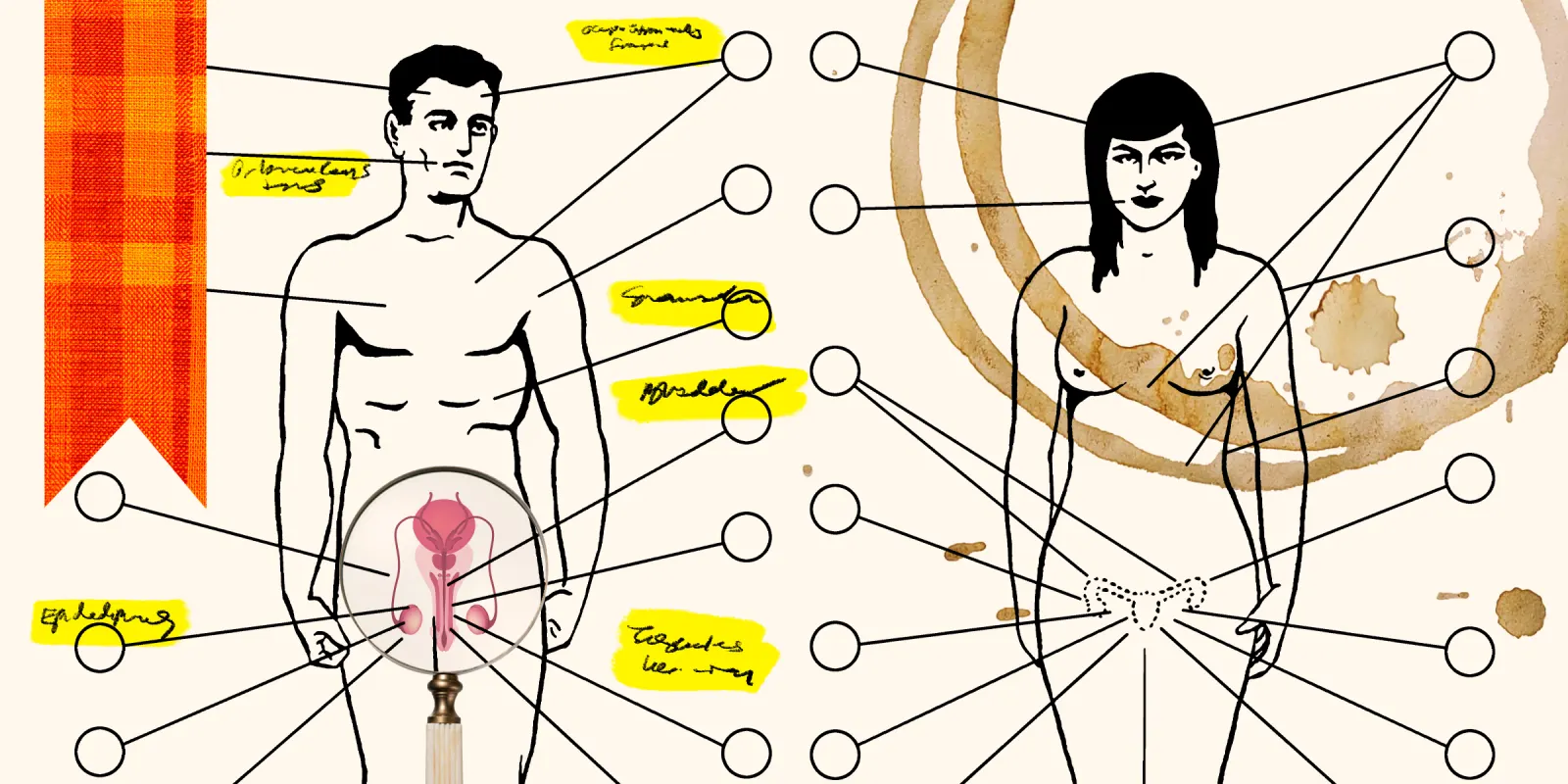
When I look back at my medical school anatomy textbook (Clemente), there is an incredible bias toward male anatomy. Medical education has consistently emphasized female reproductive anatomy and ignored vulvar anatomy, particularly clitoral nerve anatomy. This is a clear indication that medical education has historically seen women as “baby machines” and not as sexual beings. There has been a systemic disregard of anatomy critical to a woman’s sexual function.
This is exemplified in my textbook, where all the basic depictions of the pelvis are male. It is notable that there are 20 illustrations of the male pelvis and only 15 of the female pelvis. Moreover, while there are 15 detailed illustrations of penile anatomy, there are none of the clitoris. Conversely, there are seven illustrations devoted to the female reproductive system.
Fortunately, there has been a recent awakening in the medical establishment, with several publications of detailed vulvar anatomy. Yet bias dies slowly, particularly in medicine.
Human anatomy is foundational to medical education, yet detailed vulvar anatomy is still absent from first-year anatomy in many medical schools. The reasons for this are complex, but it is reasonable to speculate it is partially due to male domination of medicine until very recently.
Study of female vulvar anatomy is still absent from operative anatomy in many plastic surgery and ob/gyn residency training programs. Thankfully, there has been a “top-down” effort to encourage this critical teaching. The American Board of Plastic Surgery has added questions of vulvar anatomy to their inservice examinations, Board examinations, and continuing medical education. The American College of Obstetricians and Gynecologists has proceeded similarly.
Aside from simple equity, there are many reasons for doctors to learn female vulvar anatomy.
1) Understanding pelvic pain: There are estimates that about 25% of women of child-bearing age have chronic pelvic pain. Treating pelvic pain obviously must be based on sound anatomic training.
2) Sexual dysfunction: Worldwide, 20% of women suffer from dyspareunia and 30% of women attempting to conceive experience sexual pain, yet 70% fail to discuss it with their physician. Thus, understanding vulvar anatomy is critical to enhancing female sexual and reproductive health. Ignorance by physicians encourages physically based sexual dysfunction to be dismissed as purely psychological.
3) Female genital rejuvenation: Female genital cosmetic surgery is the fastest growing area in cosmetic surgery, with over 25,000 cases in the U.S. in 2023. Without rigid educational standards, irreparable injuries can be expected to become prevalent.
4) Female genital trauma: Though significant vulvar injuries from trauma and obstetrics are uncommon, inadequate treatment can have devastating sequelae. On a global scale, WHO estimates 200 million women have experienced female genital mutilation and there are still 3 million a year at risk. This latter group can expect restoration only if knowledge of vulvar anatomy is pervasive and detailed.
5) Transgender care: Though a controversial area, estimates of those seeking transgender care in the U.S. approach 1 million. In order to address issues of transitioning, it is vital that PCPs have a comfortable knowledge of vulvar anatomy.
Medicine is slowly evolving toward improved care specific to women, whether in the field of cardiovascular disease, mental health, or sexual health. Medical students, resident trainees, and those in practice need to demand improved training in vulvar anatomy so we can provide better care to our female patients.
Dr. Paul Pin is a plastic surgeon in Dallas, TX, and is affiliated with Baylor University Medical Center. He received his medical degree from Duke University School of Medicine and has been in practice 36 years. He specializes in aesthetic/cosmetic plastic surgery and breast reconstruction and is experienced in facial plastic and reconstructive surgery, cosmetic surgery, breast reconstruction, breast surgery, and cosmetic/aesthetic surgery.
Collage by Jennifer Bogartz / CSA Images / Getty Images