Every few weeks it seems an email appears in my work inbox announcing a shortage of another vital drug at my institution. As physicians, we are keenly aware of our access to medications. We are sincerely mindful of our patients’ barriers. We are ardently striving to provide high quality care within the confines of an increasingly limited system. Currently, the FDA reports 142 medication shortages, including anesthetics, anti-diabetics, ophthalmic drops, antibiotics, and anti-cancer drugs. This number fluctuates annually; however, only recently has the upward trajectory caught the attention of lawmakers.
Why are we struggling now? Well, truly, the shortages have been noted for at least a decade. Yet, drug supply chains were more noticeably disrupted in these past few years, resulting in a long list of rationed medications. On the supply side of this problem, multiple factors are likely to blame. One part of the issue arose in the wake of the pandemic when global supply chains shut down, hindering production. Nevertheless, Michael Ganio, director of the American Society of Health-System Pharmacists (ASHP), argued that this halt did not independently cause the current situation. He concedes that quality checks on the manufacturing side of certain drugs probably contributed more to the systemic slowdown than shipment. The tight restrictions and prolonged approval processes in the FDA hinder distribution. Moreover, when these checks disrupt production, large hospitals and outpatient care centers receive advanced notice of upcoming shortages and may “panic buy” an overstock of a necessary drug to prevent a scarcity at their institution. Despite these findings in the manufacturing process, lawmakers continue to express concern that supply shortages derive from our nation’s dependence on foreign production. FDA Commissioner, Robert Califf, MD, counters this viewpoint, stating that the falling local price of certain generic drugs and high cost of local production forces the manufacturers of these medications to seek cheaper alternatives abroad. This exodus of businesses may play some role in altering the supply chain, but it is unlikely to contribute as significantly to the underlying cause of these shortages as the process of quality checks.
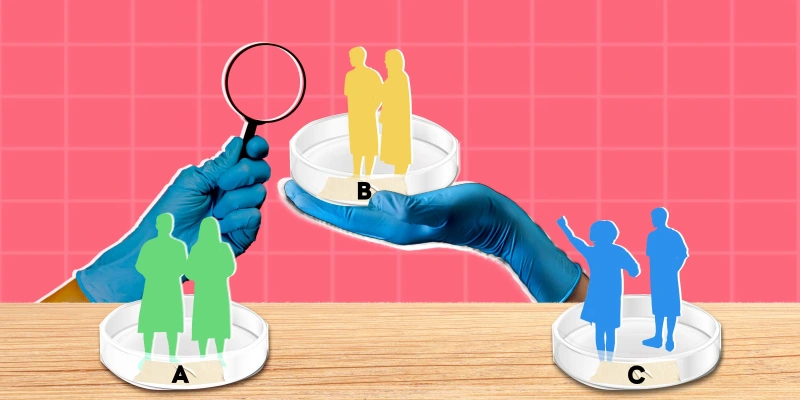
On the consumer side, the vastly increasing demand for specific drugs has led to an astounding imbalance of availability. Those drugs highest in demand include stimulants for treatment of ADHD, repurposed anti-diabetics for weight loss, and antibody treatment for RSV. When these demands outpace supplies, consumers — both health care workers and the patients they serve — are forced to search for alternative therapies or, if available, front higher costs for medications. Often, these substitutions are “second line” and therefore may be less effective or carry a higher risk of adverse effects. In 2011, a retrospective JAMA article found that shortage of norepinephrine led to increased rates of death due to septic shock when it was substituted or supplemented by phenylephrine or dopamine. Another workaround for demand-side shortages is the concept of large-scale compounders. These companies circumvent FDA regulation, producing medications at lower costs than standard pharmaceutical companies. How is this possible? The companies essentially function as a “mega-pharmacy” in which they scale up the work your local pharmacist provides to an individual who requires a special solution of a medication to suit specific patient needs.
Recently, the Biden administration presented a plan to bolster the supply of medications to combat these rampant shortages. The most notable aspect of this plan aims to generate a robust homegrown supply chain rather than relying on heavy importation of medication. This coin is two-sided. To an extent, the expansion of domestic medication production may, as intended, aid in the generation of a local drug supply. Nevertheless, some argue that even with greater supply, lawmakers will still fall short of their goal to increase medication stock in the hands of consumers unless they simultaneously downgrade the regulation of drug production. Although the concept of easing regulation sounds potentially harmful, truthfully, according to Ganio, “with our [current] FDA system of pass-fail approval, we have to assume everything is equal.” This consideration implies that the difference between a name-brand pharmaceutical company and a generic brand may be equivocal, and quality lapses may occur at any level in the chain.
In my world, the ophthalmic world, some notable shortages in eye drops have persisted through the pandemic. Some of these drops include topical antibiotics, dilating drops, and glaucoma treatments. In a 2021 letter to the editor, ophthalmologists from Bascom Palmer Eye Institute noted that prior to the pandemic, 13 drops were found on the shortage list, except for timolol, a glaucoma medication, added during the pandemic due to likely supply chain disruption. They argued that while patient care would overall remain unaffected in the short-term, long-term effects of shortages could lead to significant repercussions for patients who depend on chronic treatments. This concepts holds true for systemic medications as well.
Shortages threaten our ability to effectively carry out lifesaving and vision-saving care. While new legislation by the Biden administration may assuage the current crisis, it is unlikely to singlehandedly resolve the root cause. As physicians, it remains our responsibility to advocate for solutions that will improve patient care, and, in the interim, to execute our duties to the best of our abilities with whatever resources we may find at our disposal.
Dara was a 2020–2021 Doximity Research Review Fellow.
Image by Alphavector / Shutterstock