The following represents a fictional account of a common situation.
Mr. Barstow arrived in our Emergency Department late on a Tuesday evening. His motor vehicle collision has sent four patients to the trauma bay. Mr. Barstow was the most acute: his femur was fractured, along with an unstable burst fracture of his L2 vertebra. He was hypotensive, but a little volume resuscitation took care of that. Our level one trauma center, an academic safety-net hospital, stabilized him and got him into the trauma ICU as they had done with thousands of patients in the past. He was evaluated by Orthopedics and Neurosurgery, who determined both his leg and back would need surgery.
The neurosurgery team would plan on an open spinal fusion the next morning. He was neurologically intact, so there was no reason to take a hemodynamically unstable patient to the OR for a four-hour surgery in the middle of the night. Surgical fusion of the spine is a complex case with instrumentation, fluoroscopy and a potential for large blood loss, not a task for the night-time OR team unless necessary. The orthopedics team would fix Mr. Barstow’s femur after his spine was stabilized. Everyone agreed on the plan and Mr. Barstow was booked for the morning.
Unfortunately for Mr. Barstow, Ms. Stevens and Mr. Brooks both had elective surgeries scheduled the next day. Ms. Stevens had bad cervical myelopathy, progressively losing the ability to walk. She waited five months to be seen, as we are the only Neurosurgery clinic in this half of the state of Louisiana that takes Medicaid. Her surgery, while elective, could not be delayed much longer. Mr. Brooks, similarly, waited too long to be evaluated for his brain tumor. He also needed surgery.
Our hospital, being a safety-net facility, only has one attending neurosurgeon to cover the day’s cases. It also has a back-log of patients needing surgical care that stretches three months out. If our team isn’t allowed to run overlapping rooms, Mr. Barstow’s case must wait until the end of the day. It’s highly likely that he won’t even get surgery without us cancelling an elective case. However, allowing us to run overlapping rooms with one staff neurosurgeon (assisted by a few residents) would ensure all the patients receive the care they need. It will get Mr. Barstow’s spine stabilized so orthopedics can take care of his leg, getting him mobilized, fed, started on chemical DVT prophylaxis and on to his next phase of care. Waiting for available OR time to present itself would leave him susceptible to hospital acquired infections, DVTs, malnutrition and a host of other preventable problems. Running overlapping rooms allows all the patients to receive timely surgical care.
However, running overlapping rooms is a controversial policy. Research has shown, in multiple studies, that patients operated on in overlapping rooms suffer no worse outcomes than those operated in non-overlapping rooms. Despite this, many hospitals have banned the policy. The Senate Finance Committee even met to discuss if it should be banned nationally. While not federally banned, it is still being debated. Thinking of how that policy would affect how we care for patients like Mr. Barstow led me to my research.
I was fortunate enough to present my findings at the 2018 American Association of Neurological Surgeons (AANS) Annual Scientific Meeting in New Orleans. The talk was given the Robert Florin Socioeconomic Abstract Award. Our hospital did not always explicitly allow overlapping rooms, so we compared how we took care of these urgent cases like Mr. Barstow both before and after the policy switch (see Figure 1). These patients, it turns out, receive surgery two days quicker and have their length of stay reduced by six days when we are allowed overlapping surgery. They also have significantly lower medical complications (hospital acquired infections, DVT, etc) and a significantly higher chance of being discharged to home. The surgical complications and 30-day readmissions were equivalent between the two groups, again suggesting that there is no increased risk to these patients by allowing surgeons to operate in overlapping rooms.

From an economic standpoint, allowing overlapping rooms also makes sense. Not only did the patients in our overlapping group cost about $50,000 less per admission, their increased rate of discharge to home meant they were using fewer post-acute care resources as well. Because of our safety net status, over 80 percent of these patients were being funded with public money: Medicare, Medicaid or uninsured (which is reimbursed by the State of Louisiana). With exponentially rising health care expenditures across the country, we should embrace policies that reduce costs.
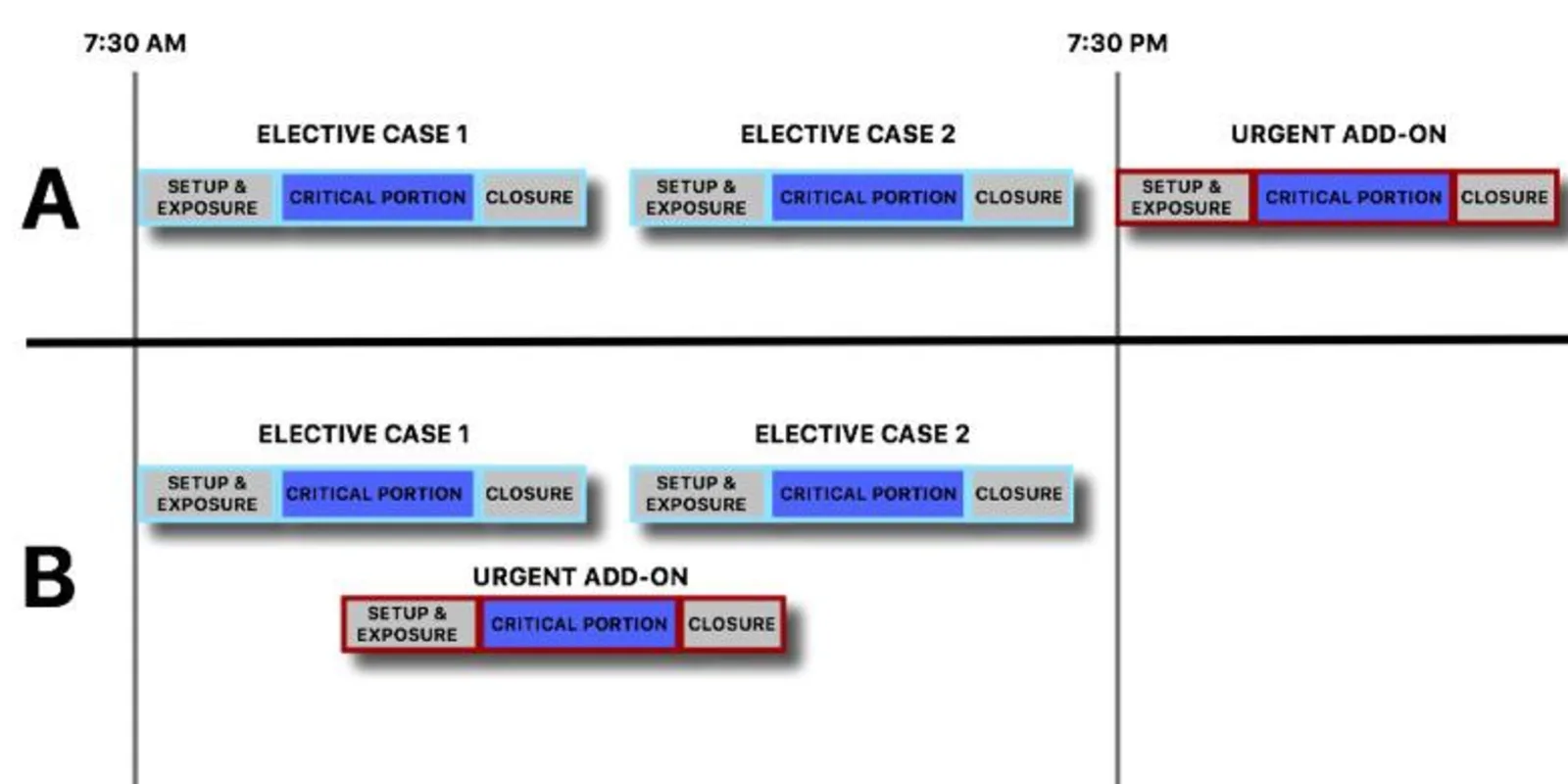
In addition, an attending neurosurgeon’s time is a valuable (and expensive) resource. By allowing overlapping rooms, this resource is utilized more efficiently. In efforts to improve resource utilization, Lean methodologies utilize time-driven-activity-based-costing. With this, efficiency is improved by ensuring that personnel work near the “top of license.” In an academic institution with resident support, an attending neurosurgeon spends more time at the “top of license” with overlapping rooms. With this policy, as per American College of Surgeon’s guidelines, the critical portions of the cases are not to overlap. This means the non-critical portions, such as exposure and closing, can be performed by residents, freeing up the attending surgeon to go between the critical portions of cases. In a non-overlapping scenario, a smaller percentage of the attending surgeon’s time is utilized at the “top of license,” since the attending still must be present for the non-critical portions of the case. (This can also be visualized on Figure 1.)
While the debate around overlapping surgery continues, it is important to keep these results in mind. Overlapping surgery is not a way for surgeons to increase their revenues. These are vulnerable patients who need surgical care. Overlapping surgery allows us to treat them in a safe, efficient, timely and cost-effective manner.
Anthony DiGiorgio, DO MHA is a Neuroglogical Surgery resident at Louisiana State University.